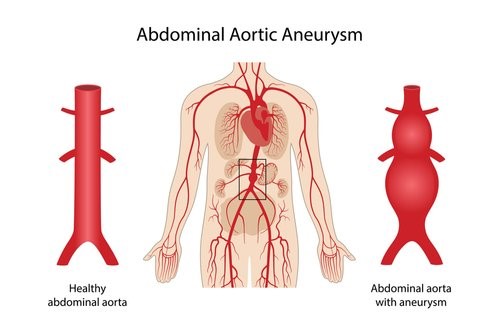
What is an Abdominal Aortic Aneurysm (AAA)?
The abdominal aorta is a large blood vessel found in the abdomen. It is the continuation of the main blood vessel (the thoracic aorta) which comes directly from the heart and travels just in front of the spine all the way down into the pelvis. Along its course, the abdominal aorta gives critical blood supply to all the organs in the abdomen, such as the liver, pancreas, kidney, spleen, and intestines.
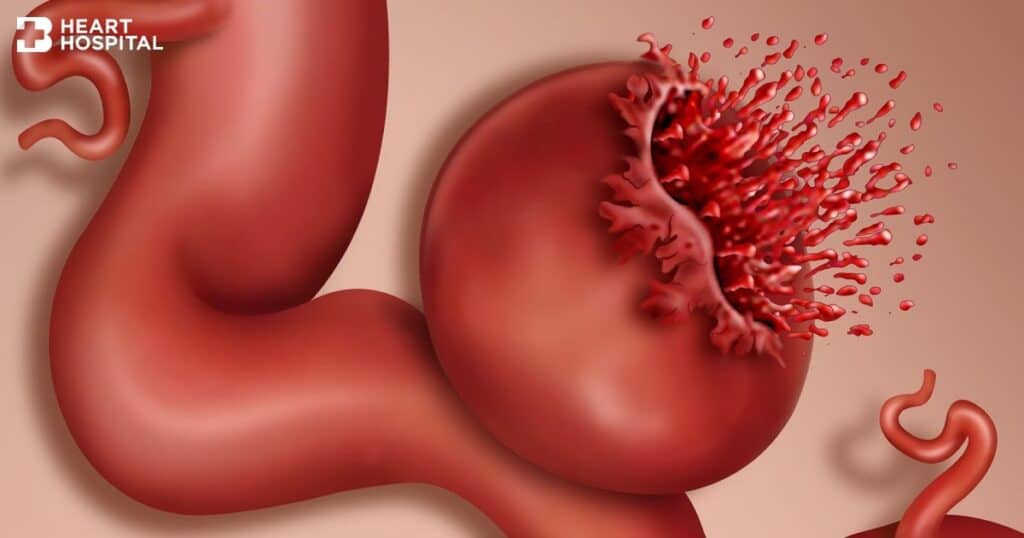
An abdominal aortic aneurysm (AAA) is an enlargement/ballooning of this critical blood vessel when a segment of its wall is weakened/damaged. Just like a balloon, when the enlargement of the abdominal aorta reaches a critical size, it can burst resulting in massive blood loss and an almost 90% rate of mortality (death).
(Source: https://www.vascularcures.org/abdominal-aortic-aneurysms)
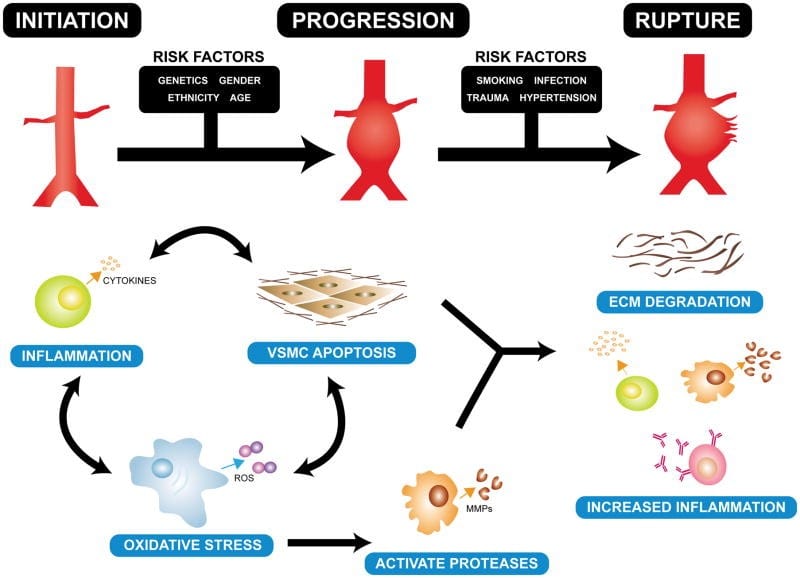
Causes and Risk Factors for developing an AAA
A combination of inflammation and cell destruction leads to loss of fibers in the wall of the abdominal aorta, thus resulting in weakening of the wall and an AAA formation. Non-modifiable risk factors for developing an AAA include:
- Genetics (if there is a related family member with the disease such as a sibling or a parent)
- Gender (males are found to be at higher risk of developing an AAA)
- Age (the risk is increased with advanced age, with the peak incidence in those aged 65 years and older)
There are also modifiable risk factors for developing an AAA, which if avoided, can significantly reduce the risk of developing the disease. Some of the modifiable risk factors include:
- Smoking/tobacco use (current smokers have a 5-fold increased risk for developing an AAA and past smokers a 2-fold increased risk as compared with non-smokers)
- High blood pressure (for every 10mmHg rise in blood pressure, studies have shown a corresponding 20% increased risk of developing an AAA)
- High cholesterol (increased levels of bad LDL cholesterol and total cholesterol levels were found to be associated with an increased risk of an AAA)
(Source: Kuivaniemi H, Ryer EJ, Elmore JR, Tromp G. Understanding the pathogenesis of abdominal aortic aneurysms. Expert Review of Cardiovascular Therapy. 2015 ;13(9):975-987. DOI: 10.1586/14779072.2015.1074861. PMID: 26308600; PMCID: PMC4829576.)
How do I know if I have an AAA?
Unfortunately, the majority of AAAs remain asymptomatic (i.e. no signs or indications) until they rupture, and the chances of survival at the point rupture is less than 10%. Thus, it is strongly advised to have screening tests to detect any underlying AAAs before the onset of any symptoms. This is especially true for individuals with any of the above risk factors.
The Ministry of Health in Singapore recommends males above the age of 65 especially those who are current or past smokers to have an ultrasound screening test of the abdominal aorta to detect the presence of any AAA.
Late symptoms of fast-growing AAAs or those with impending rupture include severe abdominal pain or lower back pain, or sudden onset giddiness/fainting. Immediate urgent medical attention should be sought for such symptoms should they occur.
How is an AAA diagnosed?
As most AAAs remain asymptomatic (i.e. no signs or indications) in the early stages, they are frequently detected incidentally (accidentally) by a scan of the abdomen done for other purposes. Unfortunately, a good majority of AAA cases are not detected early enough before they rupture, and only discovered post-mortem after the person has passed away. It is thus imperative that individuals (especially those with risk factors detailed above) undergo screening tests to check for the presence of an AAA.
Screening for an AAA is simple and non-invasive. It involves a duplex ultrasound scan of the abdominal aorta after a period of overnight fasting. If the ultrasound scan is suggestive of an AAA, a more detailed CT scan will be ordered to further define the anatomy and to plan for any treatment necessary.

(Source: https://thoracickey.com/abdominal-aorta/ )
The treatment of AAAs largely depends on the size of the AAA and whether there are any symptoms. Only AAAs smaller than 5cm in diameter and without any symptoms can be managed without surgery as the risk of rupture for these situations has been shown to be very minimal.
| AAA diameter (cm) | Yearly rupture risk (%) |
| 3.0-3.9 | 0 |
| 4.0-4.9 | 1 |
| 5.0-5.9 | 1-10 |
| 6.0-6.9 | 10-22 |
| >7.0 | 30-50 |
Non-surgical management of AAAs involves avoiding all the possible risk factors such as smoking avoidance/cessation, controlling high blood pressure, and taking any necessary medications for high cholesterol.
For patients with a AAA diameter of >5.0cm or with symptoms suggestive of impending rupture, such as severe abdominal/back pain, surgical repair should be considered to avoid the potentially fatal consequences.
What are the surgical options for AAA in Singapore?
Surgical repair of an AAA can be broadly classified into either open surgery or endovascular (minimally invasive) surgery. Open surgery for AAAs has been available since the 1950s and has seen some minor refinements to the technique since that time. In contrast, endovascular surgery (EVAR) for AAAs was first developed in the 1980s but has seen significant changes to the technique and the technology of the devices used over the years and has slowly been able to achieve similar outcomes to open surgery for a good number of cases.
Despite its promise of small scars and lesser bleeding, endovascular surgery has not been able to completely replace open surgical repair as the gold standard operation for AAAs. There remains a good number of situations where open AAA surgery still produces superior results as compared with endovascular repair, and the decision between which technique is more suitable for the individual patient depends on several factors:
- Overall fitness of the patient (namely the fitness of the heart and lung functions)
- The anatomy (morphology) of the AAA and how close it is to the important branches of the abdominal organs
- Patient preference
My surgeon has advised that I undergo open AAA surgery. What can I expect?
Open repair of an AAA if done properly, produces excellent long-term results without the risk of recurrence, and without the possible need for revision surgeries in the future. It is however considered a major operation and is not suitable for frail patients with multiple chronic diseases (e.g. heart failure, chronic obstructive pulmonary disease).
The surgery is performed under general anesthesia, where an incision will be made over the abdomen to access the abdominal cavity. The small intestines are swept to one side and the covering over the back of the abdominal cavity is opened to expose the AAA which lies just anterior to the spine.
A clamp will have to be applied to temporarily stop blood flow in the segment of aorta to be repaired, and this clamp can put a strain on the heart leading to a heart attack in patients with significant underlying heart problems.
The diseased segment of aorta is opened longitudinally (along its long axis) and a synthetic graft (made from polyester) is sewn in place to allow blood to flow from the normal segment of aorta above, to the normal segment of artery below and thus bypassing the weakened AAA segment. The small intestines are then replaced, and the abdominal incision repaired. Altogether an open AAA surgery can take anywhere from 4-8h depending on the complexity. Post-operatively, the patient will need to spend a couple of days in the intensive care unit (ICU) to monitor for any complications such as heart failure or kidney failure, before moving to the general ward. Most patients can expect to discharge from hospital about 1-2 weeks after the operation and continue light activities for a further couple of weeks before returning to their usual lifestyle.
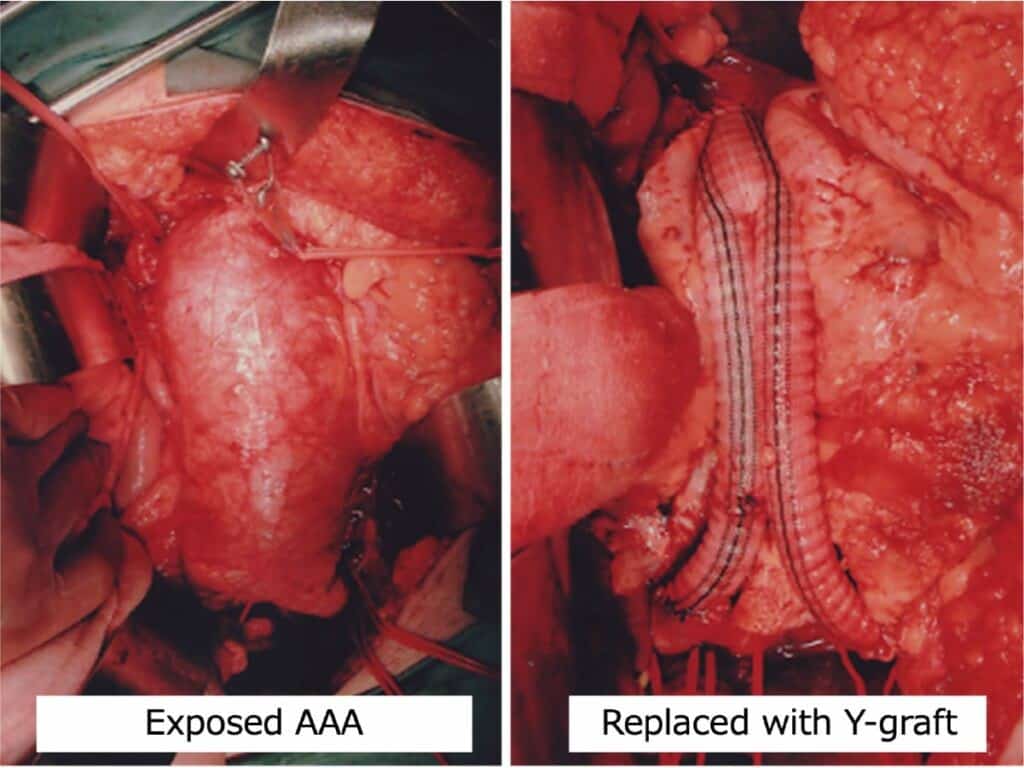
(Source: https://vascular-1su.jp/en/clinical/abdominal-aortic-aneurysm/)
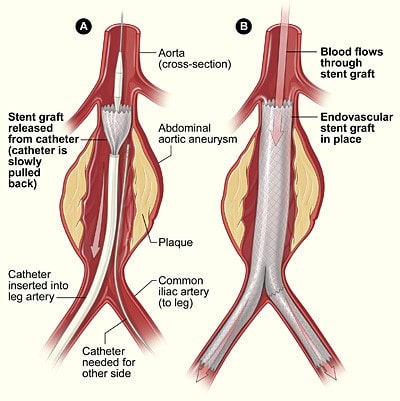
How is endovascular repair of an AAA (EVAR) performed?
Endovascular surgery for an AAA (also known as endovascular abdominal aortic repair, EVAR) can be performed under local anesthetic and sedation, as the surgery typically only involves two small 1cm punctures in both groins to perform. This makes it more suitable for patients who are frail and who may not be very fit for general anesthesia.
A device known as an aortic stent is introduced via the groin punctures and advanced upwards to the area of the AAA. Accurate positioning of the aortic stent is then confirmed using X-rays as well as special dyes injected into the blood stream. The stent is deployed to exclude the diseased AAA segment from the main circulation pathway and prevent further flow of blood into the AAA. Overtime the AAA is expected to stabilize and not expand further thus removing the risk of a fatal rupture.
An EVAR operation typically takes around 1-2h to perform, and the patient would then be expected to recover overnight in a high dependency unit before being transferring to the general ward. Most patients can discharge 1-2 days after an EVAR operation with light activities advised for a minimum of 2 weeks before returning to their usual lifestyle.
Despite its many advantages of being a minimally invasive (“keyhole”) operation with lower operative risk and quicker recovery time, EVAR is prone to stent device malfunction leading to what is known as endoleaks. Endoleaks occur when, despite the placement of the endovascular stent across the AAA, blood continues to leak into the AAA causing it to further expand and eventually rupture.
Endoleaks do not occur in every case, and some endoleaks (like the type II endoleak) can on many occasions seal itself off over time. International guidelines stress the importance of regular surveillance scans after an EVAR operation to monitor for the occurrence of any endoleaks, and for early revision surgery to repair them if present, so as to avoid a fatal AAA rupture.
(Source: https://en.wikipedia.org/wiki/Endovascular_aneurysm_repair)
Preparing for AAA surgery
Adequate preparation before AAA surgery is vital to minimize risks and ensure good outcomes. Pre-operative evaluation typically involves a detailed medical history and physical examination to detect any underlying diseases which may increase the risk of the operation. Baseline blood tests, a chest X-ray and an ECG are performed, as well as an evaluation of the fitness of the heart function. This typically involves at least an ultrasound scan of the heart. The patient will also need to be assessed by an anesthetist and any other specialist deemed necessary (such as a cardiologist or respiratory physician) prior to the surgery.
Risks and complications of AAA surgery
The risks and potential complications of AAA surgery largely depends on whether it is an open surgical repair or an endovascular surgical repair (EVAR) of an AAA. Open surgery generally carries a greater risk of stroke, heart and lung complications from the general anesthesia, as opposed to endovascular surgery which can be performed under local anesthetic.
Risks common to both include:
- Blood loss
- Infection (both implant and wound infection)
- Clotting (thrombosis) of the blood vessels supplying the legs and the abdominal organs (kidneys, small intestine etc.)
- Kidney injury
Repair of an AAA is considered a major surgery and meticulous pre-operative planning, intra-operative technique and post-operative care is essential to minimize all the potential risks of the surgery and to ensure good outcomes.
Prognosis After Treatment of AAA
An AAA is not a cancer, but there are still risks of recurrence of the condition, thus it is highly recommended to adhere to the surgeon’s post-operative surveillance recommendations. Certain situations which may increase the risk of recurrence include:
- Endovascular repair (EVAR) instead of open repair
By nature of the operation, EVAR is prone to device malfunction leading to what is known as endoleaks. Endoleaks occur when, despite the placement of the endovascular stent across the AAA, blood continues to leak into the AAA causing it to further expand and eventually rupture. Patients who have undergone an EVAR operation require lifelong surveillance to detect and treat any endoleaks should they occur.
2. An AAA involving the arterial branches to the abdominal organs
It is technically more difficult to repair an AAA which involves the branches to the abdominal organs such as the kidneys, liver and small intestines, as these branches need to be preserved during the repair. Such a surgery is unfortunately not as robust as one which does not involve these vessels and is prone to increased risk of recurrence/endoleaks.
3. Genetic predisposition coupled with non-compliance to lifestyle modification advice
Having a family history of aortic aneurysms or a genetic connective tissue disorder increases the risk of developing aneurysms in any of the other arteries in the body. Even after an AAA repair, someone with a family history of the disease can develop new aneurysms at other sites which have not been operated on. This risk is further worsening if the person continues to smoke or does not optimize their blood pressure control.
Post-Treatment Care
After undergoing AAA repair surgery, patients should adhere to follow-up appointments for monitoring. Lifestyle modifications such as maintaining a healthy diet, regular exercise, and managing blood pressure are crucial for recovery.
When to Seek Emergency Care for AAA
Unfortunately, the majority of AAAs remain asymptomatic (i.e. no signs or indications) until they rupture, and the chances of survival at the point rupture is less than 10%. Thus, it is strongly advised to have screening tests to detect any underlying AAAs before onset of any symptoms. Please see the above “How do I know if I have an AAA?” for screening guidelines.
Late symptoms of fast-growing AAAs or those with impending rupture include severe abdominal pain or lower back pain, or sudden onset giddiness/fainting. Immediate urgent medical attention should be sought for such symptoms should they occur.
Source: https://www.bangkokhearthospital.com/en/content/the-rupture-of-aortic-aneurysms-a-medical-emergency-that-might-lead-to-sudden-cardiac-death
Summary of key take-aways
An abdominal aortic aneurysm (AAA) is one of the causes of sudden death especially in individuals above the age of 65 years old. It is an abnormal enlargement of the large blood vessel in the abdomen (the aorta) which occurs in individuals with known risk factors.
This enlargement is unfortunately largely asymptomatic (without any signs or indications) until life-threatening rupture occurs. The chances of survival in the event of a rupture are less than 10%, thus the best course of action is for individuals at risk of the disease to screen for any AAA before symptoms occur and repair it early if detected.
AAA surgery is not a small undertaking and meticulous pre-operative planning, intra-operative technique and post-operative care is imperative for good outcomes. Choosing a center with the necessary technical expertise, equipment, and support staff is critical as a poorly performed AAA surgery can lead to significant morbidity and even mortality.
FAQs about Abdominal Aortic Aneurysm (AAA) Treatment in Singapore
An abdominal aortic aneurysm (AAA) is an enlargement/ballooning of the abdominal aorta, which is a large blood vessel found in the abdomen. This blood vessel travels just in front of the spine and gives off critical blood supply to all the organs in the abdomen. Just like a balloon, when the enlargement of the abdominal aorta reaches a critical size, it can burst resulting in massive blood loss and an almost 90% rate of mortality (death).
: Risk factors leading to development of an AAA include genetics (family history of the disease), Male gender, Age >65 years old, smoking/tobacco use, high blood pressure and high cholesterol. Avoiding risk factors and getting early screening for those at increased risk, can greatly reduce the chances of sudden death from a ruptured AAA.
An AAA which is asymptomatic and smaller than 5.0cm in diameter can generally be managed with good blood pressure control, reducing “bad” cholesterol with dietary modifications and/or medications, and avoidance of smoking/tobacco use. Once an AAA is larger than 5.0cm or starts to cause pain/discomfort, surgery becomes necessary to avoid a fatal rupture. Surgery for an AAA can be either via an open approach or a minimally invasive endovascular (EVAR) approach.
A: Things which need to be considered when choosing which surgery is most appropriate include:
1. Fitness of patient for general anesthesia, which is required for the open surgery approach. Patients who are more frail will benefit from the endovascular approach which can be done under local anesthesia.
2. Anatomy of the AAA (some AAAs which involve the arterial branches to the abdominal organs may not be best treated with an endovascular approach).
3. If the AAA is due to connective tissue disorders, an open repair will provide a more durable long-term result without the need for repeat revision surgeries in the future.
There are many more factors to consider and each surgical approach has its pros and cons. It is strongly advised to speak with a Vascular surgeon specializing in both modalities of aortic repair in order to choose the best surgical approach for your particular situation.
The recovery journey after treatment for an AAA greatly depends on which surgery was performed. Open AAA surgery generally takes 1-2 weeks longer to fully recover as opposed to the endovascular surgery recovery period, and the risks during the surgery of an open AAA repair are also generally slightly higher than an endovascular (EVAR) approach. The long-term results of an open AAA surgery is however on average better than an endovascular AAA repair. After an endovascular repair of an AAA, regular surveillance scans are required to detect any recurrence (endoleaks), which then need to be repaired early before life-threatening rupture can occur.
AAA surgery is not a small undertaking and carries with it significant risks, such as stroke, heart attack, blood loss, infection, organ damage and even mortality. Meticulous pre-operative planning, intra-operative technique and post-operative care is imperative for good outcomes, thus choosing a center with the necessary technical expertise, equipment, and support staff is critical for good results.
Only an AAA which is asymptomatic and smaller than 5.0cm in diameter can be managed with lifestyle changes such as:
1. Avoidance of smoking/tobacco use.
2. Ensuring good blood pressure control by reducing stress, engaging in regular moderate intensity exercise, and taking any medications prescribed by your doctor.
3. Reducing “bad” cholesterol in the blood stream with dietary modifications, weight loss if overweight, and taking any medications prescribed by your doctor.
Once an AAA is larger than 5.0cm or starts to cause pain/discomfort, surgery becomes necessary to avoid a fatal rupture.
The cost of repair of an AAA depends on several factors. It is a 6B-7A table code operation (depending on complexity) and thus the surgical fee can range anywhere from S$10k-25k. The implant cost range is generally between S$5k-25k (again depending on the complexity of the repair), and the cost of hospitalization (inclusive of ICU stay) can range from S$15-30k on average.
AAA repair is a medical necessity to avoid a life-threatening rupture, and most good insurance policies should have coverage for it. Patients are typically able to cover the cost of the surgery by utilizing both their Medisave entitlements as well as their insurance policies.
Our center is accredited by all the major insurance companies, and we will be happy to assist you in processing all the necessary paperwork from Medisave and your insurance policy, so that you can have a stress-free experience.
Dr Chen Min Qi Comments
When it comes to surgery for abdominal aortic aneurysms (AAA), it is not the case that minimally invasive (endovascular) approach is always best. Research has shown that in a good number of cases, the endovascular approach (aka EVAR) leads to increased risk of recurrence of the problem (endoleaks) requiring revision operations. Choose a surgeon who has adequate experience in both surgical approaches so that you can make an informed choice on the best treatment for yourself.

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
.
