Veins play a crucial role in carrying blood throughout our body. While arteries helps distribute oxygen and nutrients to the body’s cells, our veins act as the highways and roads that guide the blood back to our heart. Veins have one-way valves that let blood go in one direction, towards the heart. The circulatory system is also responsible for getting rid of toxins or unwanted materials in our body.
What are venous malformations and how do they affect the body?
A venous malformation (VM) is an anomaly in the body where veins do not develop properly. It is characteristed by enlarged and intricately tangled veins. When a venous malformation is located near the skin’s surface, it typically manifests as a maroon, blue, or purple spot. Children are born with venous malformations, and these malformations may not be immediately apparent. They might become visible later as the veins enlarge or expand. Deeper venous malformations within muscles or the body may remain undetected until a person experiences pain, swelling, and other symptoms. A venous malformation tends to grow as a child grows, and it may become more conspicuous in response to injuries or if only partially removed.
What are the different types of venous malformations?
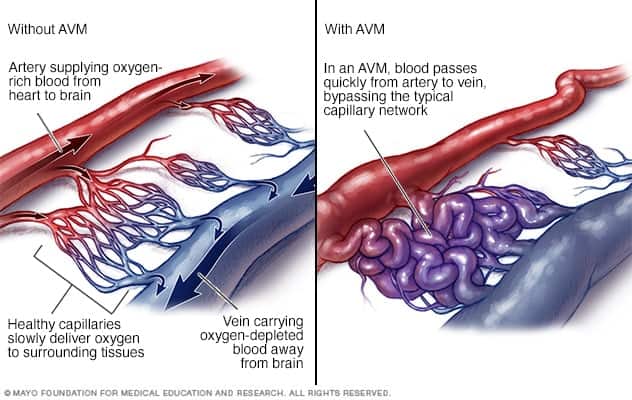
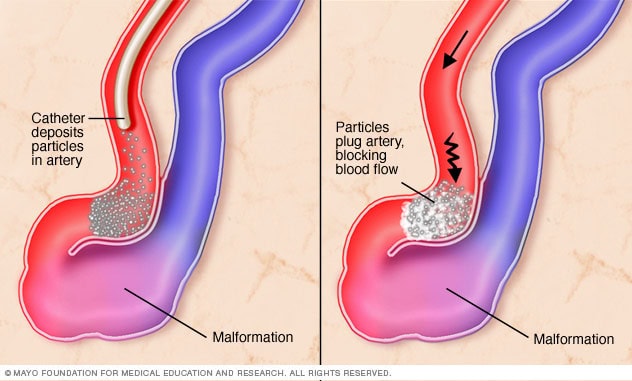
(image source: https://www.mayoclinic.org/diseases-conditions/arteriovenous-malformation/symptoms-causes/syc-20350544)
There are several types of venous malformations which can be described as:
1.Arteriovenous Malformations happen when veins and arteries grow unusually large in place of tiny capillaries. Patients with arteriovenous malformations may feel an unusual pulse in the affected area. AVMs can appear shortly before or after birth, impacting more than 1% of the population. They can replace the tiny capillaries that usually link arteries and veins, disrupting regular blood circulation. These abnormal growths are often located in the head and neck and can lead to serious issues like seizures, strokes, and breathing difficulties.
Most arteriovenous malformations don’t show any initial signs, and they can remain symptom-free for a person’s entire life. However, there’s a risk that an arteriovenous malformation might bleed, and the impact can vary depending on its size and severity. Typically, symptoms become noticeable between the ages of 10 and 40, but they can emerge at any age. Some pregnant women might experience worsened symptoms around their arteriovenous malformations due to increased blood pressure during pregnancy. Symptoms can include skin discoloration, swelling, increased vulnerability of the skin over the arteriovenous malformations leading to ulcers, and discomfort. For brain arteriovenous malformations, additional symptoms may appear, such as headaches localized to one area of the head, muscle weakness or numbness in specific parts of the body, seizures, speaking difficulties, and confusion.
The exact causes of brain arteriovenous malformations are not known, but they are believed to be congenital, meaning a person can be born with them. Some individuals may have a family history of arteriovenous malformations, although it’s unclear whether there’s a direct hereditary link. However, it’s possible to inherit other conditions that increase the likelihood of developing this type of malformation. Luckily, arteriovenous malformation treatment options are available in Singapore.
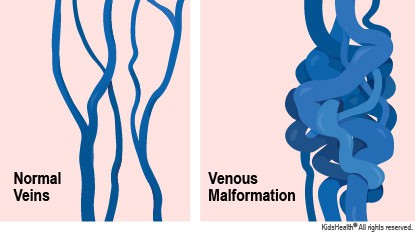
(image source: https://kidshealth.org/Hackensack/en/parents/venous-malformations.html)
2.Venous Malformations are lumps under the skin that have a bluish or skin-colored appearance. Vascular malformations can develop anywhere in the body, and the symptoms vary based on their location and type. Many individuals only become aware of these malformations and receive a diagnosis later in life, typically between the ages of 30 and 50. While some individuals, including newborns, may have these malformations from birth, noticeable symptoms tend to appear as a person gets older.
These symptoms may include visible, cosmetically displeasing growths or soft lumps that can be seen without special equipment, pain, and gradual changes in the skin’s color around the growth, and loss of limb function, which can manifest as muscle weakness, numbness, and, in severe cases, limb paralysis. If a vascular malformation occurs in the brain and is left untreated, it can lead to bleeding, resulting in a stroke or seizures due to increased pressure on the brain. Vascular malformations are typically present from birth (congenital). In rare cases, trauma can also cause vascular malformations to develop.
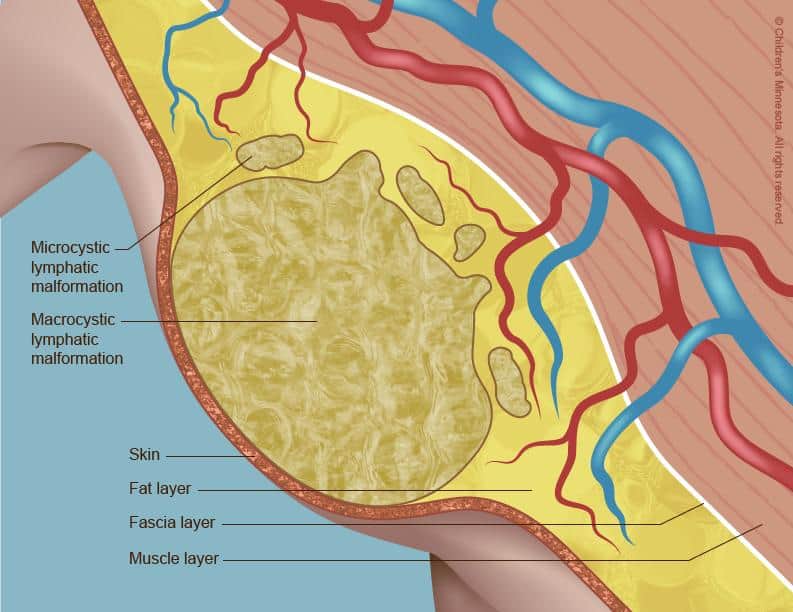
(image source: https://www.childrensmn.org/services/care-specialties-departments/fetal-medicine/conditions-and-services/lymphatic-malformation/)
3.Lymphovenous Malformations are non-cancerous masses made of fluid-filled channels. They form because the body’s lymphatic system doesn’t develop correctly. Lymphatic malformations are infrequent, benign growths characterized by fluid-filled spaces due to abnormal development of the lymphatic system. They can emerge anywhere within the body. Some superficial lymphatic malformations may resemble small, soft bumps beneath the skin, while others remain hidden from view. Irrespective of their size, these have the potential to impede nearby structures or organs’ normal function and alter the appearance of the affected areas.
Typically, symptoms arise from the compression or blockage of nearby structures, and they vary depending on the size and specific location of the malformation. Complications can arise, including recurrent inflammation or bleeding in the malformation. The inflammation results in skin swelling and redness (cellulitis). Repeated episodes of cellulitis can lead to pain and disfigurement in the affected region. Bleeding can cause intense pain, swelling, and an increase in the size of the malformation in a specific area. The development of lymphatic malformations is associated with the improper formation and development of lymphatic vessels during pregnancy.
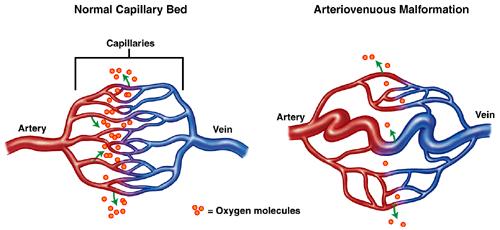
(image source: https://www.svin.org/i4a/pages/index.cfm?pageid=3316)
4.Dural Arteriovenous Fistula is a rare vascular condition that arises when abnormal connections, known as fistulas, form between arteries and veins within the protective brain covering known as the dura mater. These fistulas allow high-pressure arterial blood to flow directly into veins that typically carry blood at lower pressure. As a consequence, the brain’s venous system may become congested, potentially leading to brain dysfunction. These can be found in both the brain and the spine, and they tend to manifest later in life.
In some cases, individuals may not experience any symptoms, while others may exhibit a range of mild to more severe symptoms. A distinctive indication of dural arteriovenous fistulas is pulsatile tinnitus, a persistent whooshing sound near the ear caused by the flow of blood from arteries through the fistula into the veins.
Mild symptoms may include vision problems, eye bulging, swelling in the eye lining, while more aggressive symptoms often result from bleeding in the affected area, leading to seizures, sudden onset headaches, speech difficulties, dementia, coordination problems, and sensations of burning or prickling around the affected region. Additionally, nausea or vomiting may occur in some cases.
What is the role of vascular surgeons in treating venous malformations?
Vascular surgeons are well-equipped to diagnose the malformation’s type, size, and location through imaging techniques. The treatment would depend on your condition and the complexity of the malformation. In some cases, only a minimally invasive treatment would suffice.
Vascular surgeons carry out these procedures with precision to either block or repair the abnormal blood vessels while preserving normal function. To actively prevent further complications, vascular surgeons will also recommend having regular check-ups with you.
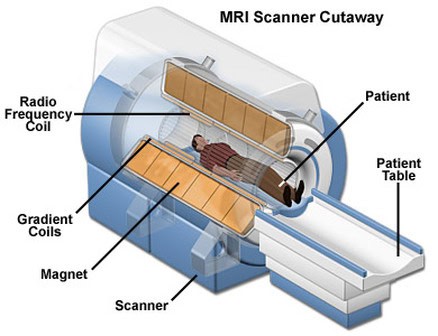
(image source: https://snc2dmri.weebly.com/components–functions.html)
How do vascular surgeons diagnose and screen patients for vascular malformations?
Diagnosis typically involves a clinical examination, and further imaging tests like computerized tomography scans (CT scans), magnetic resonance imaging (MRI), magnetic resonance angiography (MRA), and cerebral angiograms (also referred to as digital subtraction angiography or DSA) might be conducted. These imaging procedures help identify the malformation’s location, its characteristics, and the extent of damage to surrounding tissues. These tests are often repeated to monitor any changes in the size of the malformation.
What are the risks and complications associated with venous malformations?
While some malformations might not pose any immediate issues and can be closely monitored, many often result in pain and swelling. This condition can interfere with your daily activities. Patients with this condition can have a hard time performing basic tasks like exercise, work, or sports. Vascular malformations can cause varying levels of discomfort.
In more severe cases, large malformations can gradually lead to heart failure. Vascular malformations situated in solid organs like the liver, kidney, or uterus can disrupt organ function and potentially cause other health complications. When there are arteriovenous malformations (AVMs) in the brain or spine, they can block the flow of oxygen-rich blood to the brain. This can lead to dangerous complications like aneurysms, brain bleeds, and strokes.
(image source: https://www.drugs.com/mcd/spinal-arteriovenous-malformation-avm)
What are the various treatment options for venous malformations in Singapore?
Your treatment method will depend on the complexity of the malformation and your overall condition. One option is excision, in which the malformation is removed using traditional surgery. Depending on the malformation’s size, patients may need multiple sessions. There are also minimally invasive methods to halt the malformation’s growth. These treatments may require several sessions and are chosen based on the malformation’s size and type. Two such methods are embolization, a procedure that blocks blood flow to abnormal blood vessels effectively, and sclerotherapy, a non-surgical approach that involves injecting scarring solutions into veins or lymphatic components to shrink the problematic vessels.
What are some common misconceptions about venous malformations?
- Myth: Venous malformations are always painful.
Truth: Venous malformations don’t always cause pain; some can be painless and only become symptomatic if they grow or press on nearby structures.
- Myth: Venous malformations are always harmless.
Truth: While some venous malformations may remain benign and symptom-free, others can cause pain, functional impairment, or complications if left untreated.
- Myth: Venous malformations are contagious.
Truth: They are congenital conditions, meaning they are present from birth, and they cannot be transmitted to others through contact.
- Myth: Venous malformations do not need medical intervention.
Truth: While some small and asymptomatic venous malformations may be observed without treatment, others may necessitate medical procedures or surgery to alleviate pain, prevent complications, or improve cosmetic appearance.
- Myth: Venous malformations can only be treated with traditional methods like surgery.
Truth: Treatments for venous malformations may include minimally invasive procedures such as sclerotherapy or embolization to block or shrink the abnormal vessels, surgical excision for larger or complex malformations, or laser therapy for skin-related venous malformations.
Specific Treatment Options
The aim of treatment should be a complete and definite cure of the malformation. However, if the bleeding risk is low, the goal may be a complete cure, or the goal may be a reduction of AVM size to make definitive treatment safer, more effective, and less morbid. Several different treatment options are available to treat brain vascular malformations, including the following: Minimally invasive techniques such as embolization procedures, radioembolization, and stereotactic radiofrequency thermal ablation. Surgical removal or resection. A combination of the above treatments. Each of these treatments has its particular indications and may be more or less effective in the variety of individual malformations. It is important that a treatment plan be individualized for each patient. Coils or other materials can be placed endovascularly to occlude small blood vessels or arteries inside the AVM, decreasing blood flow through an AVM, and may sometimes result in gradual elimination of an AVM. A millimeter must be used, determining and minimizing any vascular damage to adjacent normal brain. Another minimally invasive therapy, stereotactic radiosurgery, delivers a single high-intensity beam of radiation to the AVM in the operating room. The radiation travels through normal brain tissue causing minimal damage. During this time, in the radiation oncology center after overnight fasting, a frame will be applied to your skull under local anesthetic to stabilize and make measurements of your AVM from multiple angles using the frame. Analysis has shown that as sources of technology improve, so have the patient outcomes. Throughout the history of stereotactic radiosurgery, technological advances have made radiation treatments more reliable and safer. When considering treatment for brain vascular malformations, it is important to understand that a variety of factors such as a patient’s health, age, and the specific characteristics of the vascular malformation influence the decision-making process. The chief disadvantage of stereotactic radiosurgery is the time required for obliteration. Unfortunately, a risk of obliteration-related bleeding per year, without further intervention, has been cited. It is not possible to provide a single, unchanging set of indications for stereotactic radiosurgery treatment for AVMs because the criteria for the treatment of AVMs are subject to change based on technological advances. Management decisions are largely subjective and depend on the experience of the treating physicians, patients’ wishes, and the local facilities for diagnosis and treatment. Definitive treatment, such as focused radiation or resection of the abnormal vessels, can reduce the long-term risk of hemorrhage. However, even when definitive treatment has been initiated, it may still take several years for the risk of hemorrhage to significantly decrease. So treatment every 6 months and earlier magnetic resonance imaging can evaluate whether the nidus is decreasing in size. All treatment has potential complications and associated morbidities, including stroke and other focal deficits, infection, hospital-related complications, and even mortality depending on patient choice. Management of BVMs aims to clarify whether a patient has a bleeding malformation and to estimate surgical risk. Identifying the type and extent of a brain malformation is more important for surgery than the risk of hemorrhage. Complications from BVMs could be due either to pressure on normal brain or a malformative lesion.
Embolization
Embolization is an important treatment option for many types of brain vascular malformations. Embolization means filling a blood vessel with a material to block blood flow. This decreases the amount of blood flow through the malformation blood vessels and improves a patient’s symptoms. Embolization is often used in combination with other forms of treatment. Blood vessels of brain vascular malformations are occluded by injection of glue, coils, or particles. The most commonly used material is ethylene vinyl alcohol copolymer. Other materials may be used in specific cases.
Embolization directly into the malformation is preferred; however, in complex cases, alternative routes are possible and sometimes essential. The most frequently injected vessels are the arteries, but sometimes veins can be the preferable route. Advantages of embolization over traditional surgery include: minimally invasive procedure, short recovery period, few physical limitations, and lower risk compared with conventional surgery. Embolization can be performed on outpatients. Indications for embolization of brain vascular malformations include a wide range of diseases. Embolization is very effective in certain diseases such as arteriovenous malformation. This is a result of over 50 years of improvements in embolization techniques and materials. In general, embolization is used for the treatment of a variety of vascular malformations to prevent symptoms when a more extensive form of treatment is not necessarily required or indicated.
Patient selection is important to maximize good outcomes. For instance, determining if there is an association between a brain vascular malformation and a recent seizure or when a person is no longer suitable for traditional surgery because of old age. Good outcomes may require careful patient assessment and careful pre-procedure imaging. Treatment risks should be weighed in relation to expected symptom reduction or lesion progression. The pre-procedure experience from centers tends to show results that are as good as, or better than, this. Serious complications can arise from embolization. Complications may be procedure-related, such as access-causing stroke or catheter-induced dissection. Embolization-induced infarction from unintended migration of embolization materials may also occur after embolization. Clinicians would have to weigh this against the treatment benefits in conjunction with the patient involved, including the anatomical findings. A detailed review of potential complications and their management can be found in the literature. Embolization in the presence of an active hemorrhage is associated with high rates of complications in both the short and long term. It should be postponed due to the risk of decompressing a hematoma, expanding it.
Surgical Excision
Surgical excision of the BVM is the traditional management of treatment, especially once an accurate diagnosis of the type of vascular malformation has been confirmed. Indications for surgical removal of any type of BVM are large lesions, combined lesions with symptoms, and an absence of effective techniques that can be considered in such patients. The aim of surgical treatment is the resection of the malformation that creates a mass effect over adjacent parenchyma. Lesionectomy with BVM is the most common approach. Surgeons need to resect the vascular malformation so that resolution of symptoms is achievable and the potential for hemorrhage is removed or reduced. Even in BVM patients with normal neurologic function, the traditional goal of surgical treatment is the resolution of symptoms that directly result from the BVM. The benefits of total excision of a BVM have to be weighed against the potential risks of surgery, including infection, which could cause a new neurologic deficit that is different from other malformation-induced symptoms, immobilizing headaches, and focal motor or language loss. Clinical and radiographic follow-up is critical in these patients to ensure recovery and progress. Both the preoperative management of patients with vascular malformations and their postoperative care are best performed with a multidisciplinary approach. Such an approach ensures maximum safety for patient transition from the interventional setting to an inpatient or outpatient clinical setting.
Comparative Analysis of Treatments
Arteriovenous Malformations For patients with brain arteriovenous malformations, the two most well-defined primary treatment options are embolization and surgical excision. Some will favor a given therapy, and there is no consensus on the ideal therapy for these patients. A comparative study of outcomes between these two approaches can provide a means to guide evaluation by stakeholders and patients. Embolization has the advantage of being less invasive, but has the disadvantage of the potential for AVM recurrence if the nidus cannot be devascularized. Embolization can be used for small AVMs, but may work better with medium-sized AVMs than with larger ones. When applied for symptomatic presentation, embolization usually requires more procedures for clot embolization and may lead to a higher risk of stroke. Surgical removal of AVMs has been associated with acceptable risks, given that it has the most potential to cure the AVM. The risk of perioperative stroke is increased in patients with SMA fistulae and anatomic features of the AVM. These patients can also benefit the most from surgical treatment. For larger or more deeply located AVMs, such as Spetzler-Martin grade III or IV AVMs, preoperative embolization is often performed, allowing removal of the deep venous component of the AVM to be delayed. It is recommended that every patient with an AVM be discussed in a multidisciplinary AVM conference, including neurosurgeons, diagnostic and interventional neuroradiologists, and radiation oncologists. Spetzler-Martin grade I-III AVMs can often be removed with an acceptably decreased operative risk. Spetzler-Martin grade IV and V AVMs can also be removed surgically, but due to the surgical risk, a supplement of stereotactic radiosurgery has to be discussed for partial or complete AVM obliteration. Spetzler-Martin grade VI AVMs can benefit from stereotactic radiosurgery as a first-line treatment or as a supplement to preoperative embolization. Spetzler-Martin grade VI AVMs may be managed in the same way as Spetzler-Martin grade V AVMs: microsurgical removal, partial embolization, and stereotactic radiosurgery to the residual AVM.
Embolization versus Surgical Excision
While embolization and surgical excision are both being increasingly used, there has been little direct comparison between these two methods. As a result, the “embolize and operate” strategy has been suggested. However, more direct comparisons are necessary. The efficacy of embolization is lower compared to microneurosurgical excision in DAVMs, but the safety profile is considered to be good with low mortality and morbidity. Microsurgery is more effective for treating arteriovenous malformations and venous malformations than embolization or radiosurgery. The subtotally resected brain AVM randomized trial showed that management of surgically approached brain AVM by elimination of angiographically visible nidal arteries improved the long-term results compared with embolization alone and did indeed result in a cure in 76% of the surviving participants.
Based on the known data, the choice between both treatment options should be dictated by the potential outcome improving the quality of life. If a patient has an unruptured brain AVM with seizures, surgery is to be preferred over embolization. In patients with ruptured brain AVM with focal seizures, surgery can be the method of choice to treat the epilepsy despite still being widely embolized before microsurgical resection. If a patient has massive intracerebral bleeding due to an arterial brain AVM, percutaneous embolization followed by microsurgery can reduce the blood loss and in some cases increase the probability of a successful nidal devascularization as compared to performing the microsurgery without embolization. This might result in an improved outcome for these critically ill patients. Over the last 25 years, we have learned that some patients do not recover from the residual AVM after nidal embolization, but still remain unaware. This is of major clinical importance. One has to be aware of it and has to communicate this clearly to the potential patient. Ongoing large studies will likely provide additional evidence.
Post-Treatment Care
For patients with BVMs, post-treatment care is an integral part of management that includes technical details such as imaging follow-up and monitoring for radiation therapy, as well as practical and emotional follow-up. Patients are generally followed more closely in the first months or years after an intervention and will then be asked to do imaging studies and appear in clinic at intervals prescribed specifically for their own diagnoses, according to their clinical course. Each person who undergoes an intervention, and their family, will likely have unique questions and fears related to a procedure that has never been done before for their unique condition. All patients need time and education before and after a procedure to understand what to expect from the procedure, what complications they may face, and to learn what symptoms and signs to watch for that require urgent medical attention that will bring them back to an emergency or regular health care provider for an evaluation. For some, the recovery is uneventful, and they return to all activities without assistance. For others, recovery may be more multi-faceted, including rehabilitation, emotional care, and ongoing management of symptoms. For example, some may experience depression, changes in seizures, or other symptoms post-intervention that were not present before the medical treatment. This could be due to stopping a medication because of compelling health reasons temporarily, or due to the intervention and its rapid effects on brain swelling or blood flow. Getting through this journey often takes a team that understands BVMs, including people who can help with symptoms from the brain and from the rest of the body. Hence, post-treatment care requires information exchange between providers close to the patient, and referral to the usual health care provider for long-term follow-up once the post-intervention healing is secured and maximized. This care will include consideration of lifestyle, such as a healthy diet, regular exercise, blood pressure control, smoking cessation requirements, and the use of birth control in some women.
Recovery Times
The recovery times following embolization and surgery to treat a BVM vary according to the complexity of the treatment used and the complexity of the BVM being treated. Specifics will be discussed at the time of discharge. After undergoing an embolization, the average time to recuperate and get back to normal is estimated to be a few days to a week. In general, children tend to recover faster than adults. Depending on the complexity and location of the BVM, limitations may range from 1 week to 6 weeks. After one undergoes a surgical excision, the average time to recuperate and get back to normal is estimated to be 2-3 weeks, and limitations are not usually necessary. Once children undergo therapeutic intervention, the vast majority have no limitations and go back to regular activities within a few days to a few weeks. Following treatment for a brain vascular malformation, there are no medical or surgical indications for remaining in the hospital or rehab facility. The patient should be released when it is safe to do so. They should receive a follow-up phone call the day after treatment, and an appointment should also be made for the following week at the surgical clinics or wherever a follow-up appointment is appropriate. A full evaluation will be made at the follow-up clinic to ensure that there have been no problems following treatment. Once at home, return to the hospital or emergency room immediately if there have been any of the aforementioned neurologic problems. Generally, complete recovery can be expected after a successful treatment followed by a 6-week recovery period. The patient should be fully evaluated at the appropriate clinic again at the 6-week point. If all is well at this time, they will most likely return to resume all activities, including sports.
Long-Term Outcomes
Each type of treatment option has its own unique success and failure rates. In general, long-term cures are most likely to occur with people undergoing resection of their AVM. The most extensive study looked at outcomes in about 1,500 patients followed up to 15 years. After that time, only about 7% of people had a recurrent AVM. Overall, long-term cure rates following treatment of unruptured or ruptured AVM are reported at 30-75% of those studied. Curative rates following embolization of brain AVMs are reported as 25-40%, and following radiosurgery of brain AVMs are reported at 35-85%.
Other studies report long-term cure rates after any type of brain AVM treatment at 50-80%. “Long-term” is a minimum of 3 to 5 years after treatment. There are some reports of ever-increasing numbers of cures with longer follow-up. For example, a recent study found that up to 20 years after successful AVM radiotherapy, cures continue to occur. At the end of the mildest part of the bleeding grades, those with hemorrhages tended to have mild outcomes except for dysesthesias. Maybe bad outcomes helped spur surgical treatments of those with hemorrhages earlier, where poor outcomes after hemorrhage would be less common in all comers. Because malformations may cause hemorrhage at any time, not just while waiting for intervention, progress among the no-treatment control arms would be a better gauge of the efficacy of treatment alone. However, there will be a strong tendency to treat those that decline or crossover to intervention rather than keep them in a study no more controlled. Since most interventions are not done in a major emergency, poor outcomes that aren’t significant or lethal at the time of the catastrophic event can look reasonable initially until they turn into significant disability as time goes on. Hemorrhage is immediate, and the severity of immediate consequence on top of potential later consequences factors into the common grade scales.
FAQs:
Venous malformations are abnormal collections of veins that can occur anywhere in the body. They are typically present from birth and can vary in size and appearance.
The benefits of treating venous malformations include relief from pain, improvement in cosmetic appearance, prevention of complications like bleeding or infection, and restoration of normal function, particularly in cases where the malformation affects daily life activities.
Arteriovenous malformations (AVMs) involve abnormal connections between arteries and veins, disrupting normal blood flow. They can lead to serious complications, including bleeding and neurological issues, particularly when located in the brain. Venous malformations primarily affect veins and may not always present symptoms unless they grow or press on nearby structures.
Symptoms of brain AVMs may include localized headaches, muscle weakness or numbness, seizures, confusion, and difficulties with speech. These symptoms can emerge at any age but are often noticeable between 10 and 40 years old.
The long-term impact of venous malformation treatment varies depending on the individual and the specific treatment. In many cases, successful treatment can lead to significant improvement in symptoms and quality of life, with the potential for lasting benefits. However, regular follow-up may be necessary to monitor for any recurrence or new developments.
References:
- https://my.clevelandclinic.org/health/diseases/23409-vascular-malformations
- https://www.sgvascularctr.com/tag/venous-malformations/
- https://www.stanfordchildrens.org/en/service/dermatology/vascular-anomalies/venous-malformation

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
