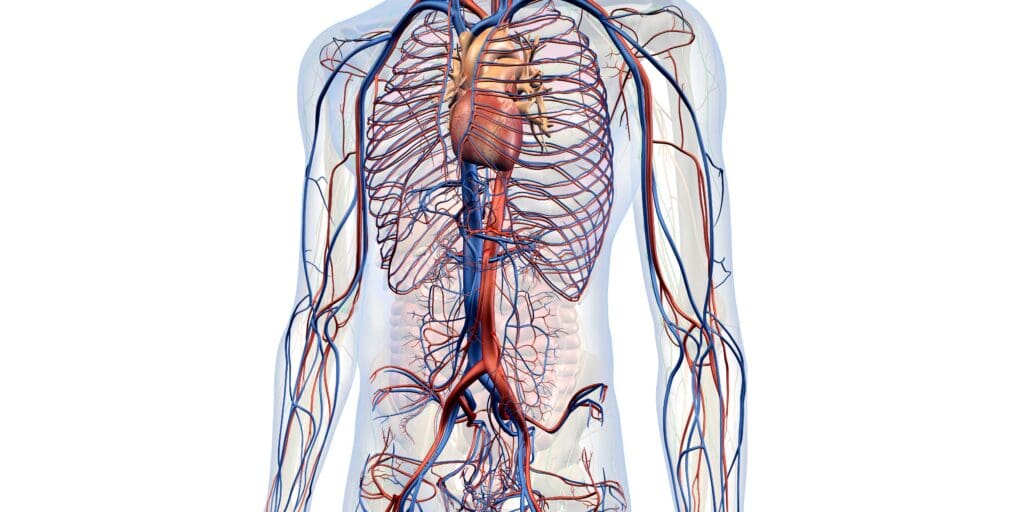
Vascular diseases are any diseases which primarily affect the blood vessels (mostly veins and arteries); they can affect people of any age. If you would like to know more about commonly seen vascular diseases, please visit this page.
Continue reading this article to find out more about the different methods of diagnosis and options for treatment, as it varies with each disease.
Types of Diagnosis and Vascular Disease Treatment Singapore:
- Peripheral Vascular Disease (PVD)
PVD is a vascular disease where arteries and veins are narrowed, due to fatty deposits hardening into plaque in the vessel walls, and causing less blood than normal to flow to the rest of the body, thus decreasing their ability to function properly.
Diagnosis
- Angiogram/Angiography
Aside from the general physical exam and taking a comprehensive medical history, a specialist will diagnose PVD by doing an ultrasound or an angiogram. An angiogram is a test where an X-ray of your blood vessels will be taken. Contrast dye will be injected via a thin and narrow tube (catheter) which is inserted into your leg to reach the targeted arteries to make the arteries visible on the X-ray. During the procedure, you will be conscious with local anaesthetic applied to the area where the catheter has been inserted. You can also opt for a sedative on top of the local anaesthetic. After the procedure, you should be able to go home within the day, though you will most likely need someone to drive you home as you will be unable to drive on your own.
Treatment
Because PVD is a marker of increased risk of a heart attack or stroke, the first objective of treatment is to reduce your risk of heart attack and stroke as much as possible. If you have been diagnosed with PVD, you are advised to exercise regularly and stop smoking if you have not done so, and you may be required to take medication to aggressively treat conditions which could accelerate the onset of atherosclerosis, such as high blood pressure and diabetes. With regards to the issue of reduced blood flow to the organs affected by PVD, there are two surgical treatment options:
- Angioplasty
A sheath will be inserted into the targeted artery via which devices will be introduced to attempt to widen the narrowed vessel. This can be done in multiple ways: a balloon and stent angioplasty involves introducing a high pressure balloon via the sheath and inflating it in the vessel to widen it, then leaving a wire mesh structure (stent) to keep it open. An atherectomy, however, would entail using a device to mechanically remove the blockage in the vessel. These are both minimally invasive procedures so you will have minimal surgical scars, and you should be able to go home on the same day or occasionally one day after the procedure.
- Vascular bypass surgery
This is an open surgery technique where a healthy vein or a plastic tube is attached from a healthy part of the artery proximally to a healthy part of the artery distally, thus bypassing the blocked segment of artery. The vast majority of people with PVD will not have to opt for this, and it is usually reserved as a second-line procedure after having undergone angioplasty or atherectomy and yet failing to improve.
DVT is a condition where a blood clot has formed in one or more deep veins (veins found deep beneath the skin, unlike superficial ones). It is considered serious because if even a small bit of the blood clot breaks off and travels upwards, it could block key arteries or veins (called an embolism). One occurrence which should be prevented at all costs is a pulmonary embolism, where the clot gets stuck in one of the arteries leading to the lungs; this impairs one’s ability to breathe properly.
Diagnosis
- D-dimer Blood Test
D-dimer is a small piece of protein formed after a blood clot dissolves
People with DVT will have abnormally higher levels of D-dimer. A D-dimer test simply needs your blood sample, so it does not need any special preparation.
- Duplex ultrasound
A duplex ultrasound uses two modes of ultrasound, Doppler and B-mode, to obtain a scan of the vessels in your body. The B-mode transducer pulls up an image of the targeted vessel while the Doppler probe evaluates the velocity and direction of blood flow in it. From this scan, it can be determined if there is a blockage in your deep veins.
Treatment
Because DVT is caused by the formation of blood clots in the deep veins, your doctor may prescribe blood thinners (anticoagulants) to prevent existing clots from enlarging and lower the risk of generating more blood clots. If blood thinners alone prove ineffective, you might be given clot busters (thrombolytics), which can cause severe bleeding. Do take note that if you are pregnant, you should not take blood thinners without your doctor’s prescription. You may also be advised to wear compression stockings to reduce swelling and the risk of blood pooling in the legs, to avoid the formation of more blood clots.
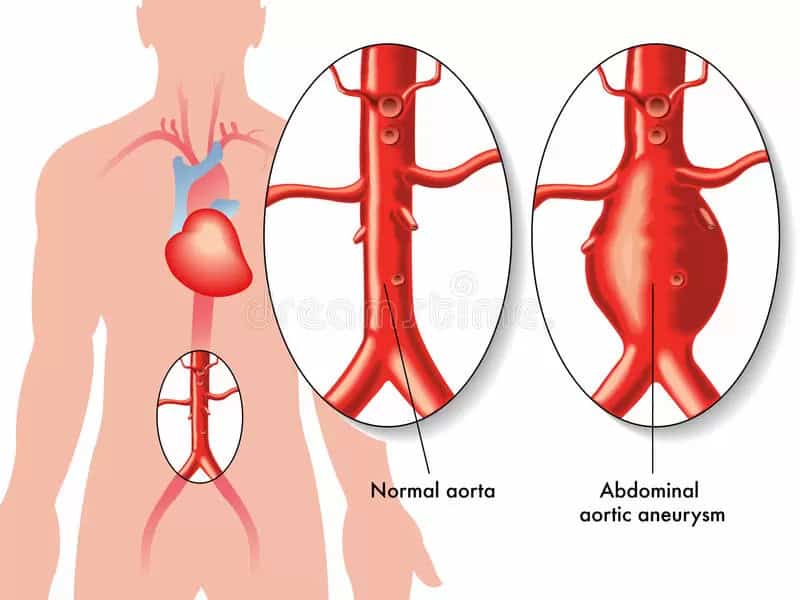
The aorta is the main artery, passing through the centre of the chest and abdomen, that supplies oxygenated blood from the heart to the rest of the body. An AAA means that a bulge has formed at the abdominal aorta, because the wall of the aorta has weakened in that area. It is in danger of rupturing and causing severe internal bleeding. The abdominal aorta is usually 2cm wide, one of the widest arteries in the body, however an AAA can cause it to expand to more than 5cm wide (when it is over 5.5cm wide it is classified as large). In the US, a ruptured AAA is the 15th leading cause of death overall, and the 10th leading cause of death in men over 55. An AAA might form because of atherosclerosis, the deposit of fatty tissue on the walls of the aorta, or high blood pressure, which weakens them.
Treatment
If the AAA is small, you will be advised to monitor it and go for regular scans, most likely every 6 months, to check that it is not growing bigger. You should also make sure that other conditions such as high blood pressure are managed well as they can worsen the condition of the AAA. However, if it is sizable enough, there are surgeries you can opt for:
- Endovascular repair
In this surgery, a catheter will be inserted through an artery in the groin and guided towards the aorta. A wire mesh tube (graft) attached to the end of the catheter will be expanded and fixed in place at the site of the AAA. The graft reinforces the weakened walls of the aorta to prevent the AAA from rupturing. After the surgery, you will most likely be required to come back for scans to check that the grafted area is not leaking. However, this surgery may not be possible for everyone, so do consult your doctor first.
- Open abdominal surgery
This is an open surgery where the weakened part of the aorta is taken out and a graft is sewn in its place. Recovery time is a month or longer.
Where should I go for vascular disease treatment Singapore?
Should you have any concerns about vascular diseases and would like to know more about options for vascular disease treatment, feel free to book an appointment with us today!
