Vascular malformations are developmental abnormalities affecting arteries, veins, and lymphatic vessels, causing diverse symptoms. Treatment involves meticulous surgery to close off abnormal vessels, often requiring multiple sessions for optimal results. This approach ensures comprehensive management and improved outcomes. Surgical intervention aims to alleviate some symptoms and address functional impairments. Understanding the importance of a personalized treatment plan is crucial for achieving optimal outcomes.
(https://www.barrowneuro.org/condition/arteriovenous-malformation-avm/)
Introduction to vascular malformation
Vascular malformations are rare developmental abnormalities involving blood vessels (arteries, veins and lymphatics), which can occur anywhere in the body. While they are typically present at birth, they may not become evident until later in life. These malformations can manifest as soft tissue masses, pain, swelling, or skin discoloration. Some occur on the face, neck, brain, or spinal cord, while others resemble birthmarks or red blemishes.
In certain cases, vascular malformations can develop in adulthood following trauma or other incidents. Treatment may be necessary for malformations causing pain, functional impairment, bleeding, or other complications. These conditions affect the vascular system, comprising veins, arteries, and lymph vessels. Rather than forming smooth networks, the vessels enlarge, tangle, or form abnormal connections, disrupting blood flow.
Vascular malformations are characterized by the abnormal growth of arteries, veins, and/or lymphatic vessels, lacking a normal pattern. Although typically non-cancerous, they can grow and invade surrounding tissues. Some types of vascular malformations are extremely rare, affecting less than 1 percent of the population. Many remain asymptomatic until triggered by factors like adolescence, pregnancy, major surgery, trauma, or injury.
These malformations result from the abnormal growth and development of a single vessel type or a combination of vessels. Over time, they can increase in size and pose varying degrees of risk, ranging from harmless and minor to severe or life-threatening.
Types of vascular malformations
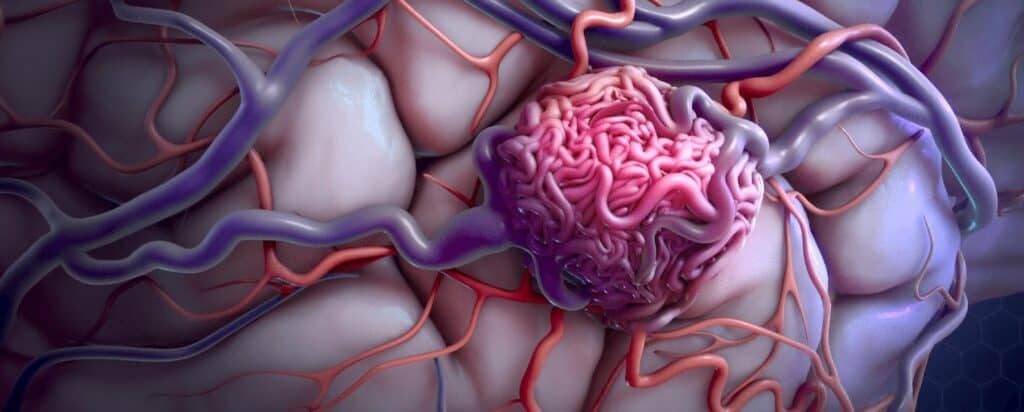
Arteriovenous malformations (AVMs) are visible abnormal growths of veins and arteries, characterized by incorrect connections between arteries and veins without the presence of capillaries. They can affect the brain or spine and may cause pulsing sensations or thrills. Venous malformations (VMs) are abnormal enlargements of veins, appearing as bluish or skin-coloured soft lumps under the skin. They are the most common type of congenital vascular malformation and can be present at birth but may not be clinically evident until later in life.

Lymphovenous malformations (LVMs) are non-cancerous masses of fluid-filled channels resulting from the abnormal development of the lymphatic system. They typically develop in the soft tissues of the face, neck, and axillary regions. Dural arteriovenous fistulas happen when fistulas form between arteries and veins in the area of the brain. Haemangiomas, on the other hand, are non-cancerous growths of blood vessels, often appearing as red birthmarks on infants and can be found anywhere on the body, commonly on the face, scalp, back, or chest.
Causes of vascular malformations
Vascular malformations are typically present at birth, resulting from abnormal development of vascular and lymphatic channels during pregnancy. Injuries or hormonal changes during puberty or pregnancy can make venous malformations noticeable later in life. In some cases, genetic mutations inherited from family members can increase the likelihood of developing vascular malformations. Certain conditions like hereditary haemorrhagic telangiectasia or Klippel-Trenaunay syndrome may be associated with specific types of malformations.
The causes of brain arteriovenous malformations (AVMs) are not fully understood, but they are believed to be congenital, and there may be a familial predisposition. However, the hereditary nature of AVMs is still uncertain. Trauma can also contribute to the development of some vascular malformations.
Lymphatic malformations occur when lymph veins do not form properly during pregnancy. The exact cause of haemangiomas, characterized by clumped blood vessels, is not yet identified. Infantile haemangiomas are more common in infants with low birth weight, premature infants, and multiple births (such as twins or triplets).
While vascular malformations are predominantly congenital, their hereditary nature is still not fully established. Trauma, genetic mutations, and abnormal development during pregnancy can contribute to the development of these malformations. Further research is ongoing to understand the precise causes and risk factors associated with different types of vascular malformations.
Symptoms of vascular malformations
AVMs are often symptomless, allowing individuals to live with them comfortably. However, there is a bleeding risk, with varying consequences based on AVM size and severity. Symptoms may arise between ages 10 and 40, and pregnant women may experience worsened symptoms due to increased blood pressure. Common symptoms include skin discoloration, swelling, sensitivity, ulcers, and discomfort.
LVM symptoms result from nearby structure compression or obstruction, varying based on size and location. Complications include recurrent inflammation or bleeding. Inflammation leads to skin swelling and redness (cellulitis), causing pain and disfigurement. Bleeding causes severe pain, swelling, and enlargement of the affected area.
DAVF symptoms can range from mild to aggressive, including pulsatile tinnitus. Other mild symptoms are vision problems, eye bulging, and eye lining swelling. Aggressive symptoms result from haemorrhages and include seizures, sudden headaches, speech difficulties, dementia, coordination issues, burning/prickling sensations, and nausea/vomiting. Note: Pulsatile tinnitus doesn’t always indicate DAVF but may indicate another condition.
(https://www.mayoclinic.org/diseases-conditions/brain-avm/symptoms-causes/syc-20350260)
Most haemangiomas are asymptomatic, except for the smooth, raised red birthmarks they cause. After disappearance, the skin may be slightly discoloured with a small persistent lump. However, some haemangiomas can bleed, develop sores, and cause pain and infection. Organ haemangiomas may rarely result in pain and complications.
Diagnosis of vascular malformations
Typically, a clinical examination is followed by imaging procedures such as CT scans, MRIs, MRAs, and cerebral angiograms when diagnosing vascular malformations. These tests determine the location, nature, and impact of the malformation on the surrounding tissue. CT scans produce detailed cross-sectional images using X-rays and computer processing, whereas MRIs use magnets and radio waves to visualise soft tissues. MRAs provide a non-invasive evaluation of blood vessels, whereas cerebral angiograms require the injection of contrast dye to evaluate blood flow patterns and precisely locate the malformation. Regular imaging helps monitor the progression of the malformation and the efficacy of treatment interventions. Combining clinical examination with these imaging techniques ensure accurate diagnosis and personalised treatment planning.
Treatments for vascular malformations
Treatment for vascular malformations typically involves closing off or surgically removing affected blood vessels, with minimally invasive techniques being effective for most cases.
1.Surgical excision of the malformation may require multiple sessions depending on its size and can recur or result in disfigurement if not completely removed.
2.Minimally invasive methods can effectively halt the growth of the malformation, with some patients requiring multiple treatment sessions based on the size and type of the malformation. These methods include:
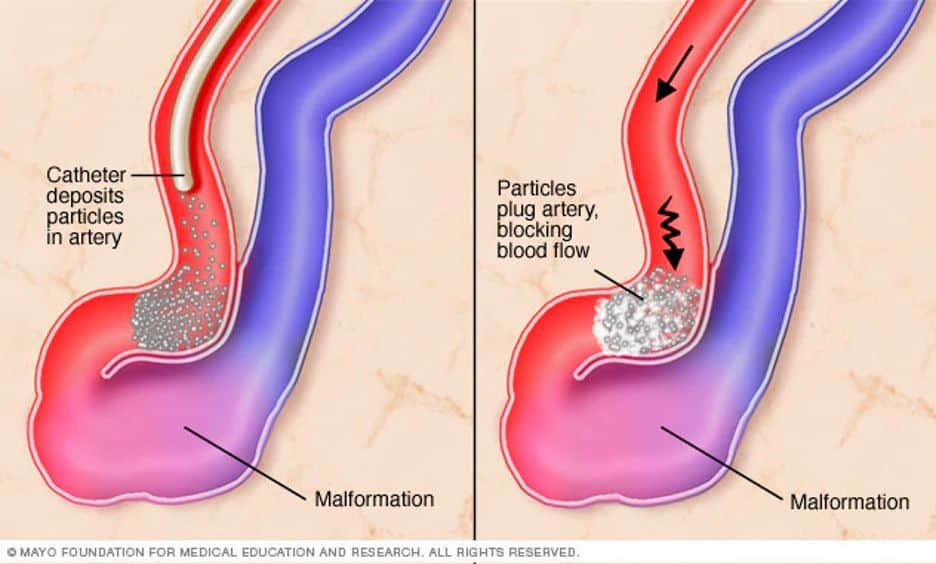
a.Embolization effectively blocks blood flow to abnormal blood vessels and treats targeted areas by blocking off malformed arteries, making it a highly successful interventional treatment.
b.Sclerotherapy is a non-surgical procedure that involves injecting scarring solutions into veins or lymphatic components to shrink blood or lymph vessels, providing an effective treatment option with just an injection.
c.While medications like propranolol and beta-blockers can resolve haemangiomas, interventional therapies offer an alternative treatment for non-responsive cases or patients seeking non-pharmacological options.
d.Laser therapy utilizes lasers to eliminate surface blood vessels and reduce lingering abnormalities caused by haemangioma, like uneven skin texture.
(https://neuroaxis.com.au/conditions-treated/cerebrovascular-diseases/arteriovenous-malformation/)
Complications of vascular malformations
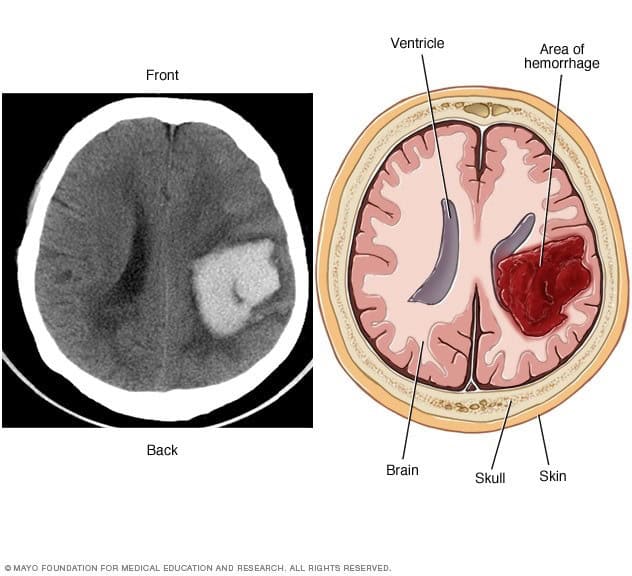
While some malformations can be observed without causing issues, others commonly result in pain and swelling, which can lead to limitations in activities like exercise or work. Large, high-flow malformations may eventually lead to heart failure. Vascular malformations in solid organs such as the liver, kidney, or uterus can cause organ dysfunction and related complications. AVMs in the brain or spine can impede oxygenated blood flow, potentially leading to life-threatening problems like aneurysms, intracranial haemorrhage (brain bleeds), and strokes. AVMs in the head and neck region are particularly common and can have severe consequences, including seizures, strokes, and breathing difficulties.
Prevention of vascular malformations
Vascular malformations are congenital conditions that cannot be prevented. Genetic counselling is recommended for individuals with a family history of related conditions to discuss options for reducing the risk of passing the condition to children. Early detection and appropriate medical care are crucial for managing symptoms and complications. Engaging with support networks and advocacy groups can provide valuable resources and emotional support for individuals and families affected by vascular malformations.
Latest advancements in vascular malformation treatment
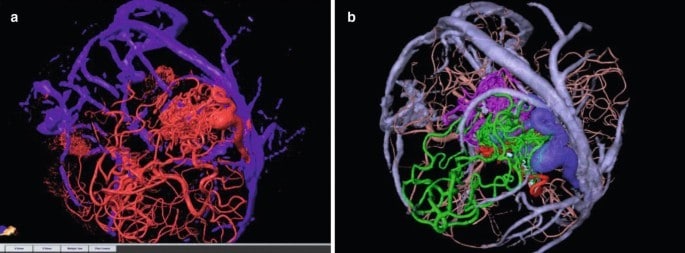
Current research focuses on improving the prediction of haemorrhage risk in individuals with brain AVMs to enhance treatment decision-making, considering factors like high blood pressure within the AVM and associated hereditary syndromes with neurological implications. Evaluation of innovative imaging technologies such as 3D imaging, brain tract mapping, and functional imaging shows promise in enhancing surgical precision and safety when removing brain AVMs while preserving surrounding vessels. Furthermore, advancements in embolization, radiosurgery, and microsurgery techniques are expanding the possibilities for surgical removal of previously deemed inoperable brain AVMs, making the procedures more accessible and safer.
(https://link.springer.com/chapter/10.1007/978-3-030-63453-7_12)
Recovery and rehabilitation after vascular malformation treatment
Overall, our minimally invasive procedures offer patients the advantage of a same-day discharge, minimal discomfort, and a swift return to their regular routines. Some cases may require multiple sessions of such surgical excision or minimally invasive procedures, depending on the complexity of the condition. While there may be temporary discomfort and swelling in certain cases, appropriate measures are taken to alleviate these symptoms and support the healing process. However, it is common to experience some degree of discomfort for some time after the procedure. It is important to note that the full shrinkage of venous and lymphatic malformations may take several weeks to occur. During this period, patients are monitored closely to ensure proper healing and progress.
Coping with vascular malformation
Vascular malformations, which can also present itself as birthmarks, can negatively impact appearance and self-confidence, leading to mental health conditions like depression and anxiety. However, most of these malformations have positive treatment outcomes. Serious malformations like brain AVMs can pose life-threatening risks if they begin to bleed. Seeking timely medical intervention is crucial for managing such conditions effectively. It is vital to consult a vascular surgeon to manage vascular malformations effectively. These specialists possess the expertise and knowledge to provide accurate diagnosis, develop personalised treatment plans for individuals affected by these conditions.
Support groups for vascular malformation patients
Birthmark Community (Singapore) on Facebook is an online support group dedicated to individuals with vascular malformations, offering a safe and inclusive environment for sharing experiences, knowledge, and mutual support. Through this community, individuals can connect with others facing similar challenges, finding solace, understanding, and encouragement on their unique journeys with birthmarks. The community fosters a sense of belonging, allowing members to exchange insights and receive empathy from those who can relate to their experiences and provide valuable support.
Common myths about vascular malformation
- It is a common misconception that all vascular malformations are harmful and require immediate treatment, whereas many are benign and do not necessitate intervention.
- Another misconception is that vascular malformations are purely cosmetic issues, neglecting the fact that they can cause functional impairments, pain, or even life-threatening complications depending on their specific characteristics.
- There is a belief that complete cure or elimination is possible for all vascular malformations, whereas treatment primarily focuses on symptom management, complication reduction, and enhancing overall quality of life rather than achieving complete eradication.
- It is a misconception that vascular malformations do not develop in later life. Hormonal changes during puberty and pregnancy can affect vascular malformations, leading to the accumulation of fluid or blood in poorly formed veins or lymphatic channels, while abnormal connections between arteries and veins can cause their manifestation later in life.
- Although surgical excision is a possible method to treat vascular malformations, it is not the only treatment for this condition. Other medical procedures such as embolization and sclerotherapy can be performed for patients with vascular malformations.
Questions to ask your doctor about vascular malformation:
It is crucial to inquire about the following aspects of your vascular malformation from your vascular surgeon to ensure a comprehensive understanding of your condition and treatment options:
- What factors contributed to the development of the vascular malformation?
- How would you classify or categorize the specific type of vascular malformation I have?
- Based on my condition, what treatment approach would be most suitable?
- What are the potential risks or side effects associated with the recommended treatment?
- How long will it take to see results from the treatment?
- Are there any specific signs or symptoms I should be vigilant about that could indicate complications related to my vascular malformation?
- How will this vascular malformation impact my health and quality of life?
- Will I require ongoing monitoring or follow-up visits after treatment?
- Can you provide me with any information or guidance on managing the emotional impact of living with a vascular malformation?
- What is your experience in treating vascular malformations, and do you have any success stories or patient testimonials you can share?
Common mistakes to avoid when dealing with vascular malformations
- Do not delay medical evaluation for vascular malformations, as prompt diagnosis and treatment are necessary to prevent complications or deterioration of the condition.
- Consult qualified vascular surgeons for an accurate diagnosis and information about vascular malformations. Do not rely on self-diagnosis or inaccurate information.
- It would be wise to consider minimally invasive procedures, surgical intervention, and targeted therapies to increase the likelihood of successful management of vascular malformations.
- Recognise and address the emotional impact of vascular malformations by seeking assistance from professionals or support groups in order to effectively manage the associated difficulties.
- Ensure long-term surveillance and follow-up for vascular malformations in order to evaluate progression, identify complications, and maximise outcomes.
What to expect when getting treatment for vascular malformations
Initially, a healthcare professional will conduct a comprehensive evaluation, including a thorough review of the patient’s medical history, a clinical examination, and imaging testing to determine the nature and extent of the malformation. Based on the evaluation, the treatment plan, which may include minimally invasive procedures, surgical intervention, or other targeted therapies, will be discussed. The duration, potential risks, and potential adverse effects of the treatment will be described in detail. During treatment, the vascular surgeon and the medical staff will prioritise the patient’s comfort and safety by administering the proper pain management methods like anaesthesia or medicine. There will be a period of recovery following treatment, which can vary depending on the nature and extent of the intervention. Appointments will be scheduled to monitor the patient’s progress, evaluate the treatment’s efficacy, and address any potential concerns or complications. Throughout the course of treatment for vascular malformations, straightforward communication with the healthcare team is essential for understanding and managing expectations and ensuring the optimal outcome.
How to stay informed about vascular malformations
The Vascular & Interventional Centre offers comprehensive care for various vascular conditions, with a team of skilled vascular surgeons specializing in endovascular and surgical treatments. They prioritize holistic care and provide integrated and personalized treatment in a comfortable environment. Equipped with advanced facilities, including a fully integrated clinic and Day Surgery Centre, the centre ensures efficient and convenient medical care. To learn more or seek assistance, contact the centre at +65 6694 6270 or email en*****@sg***********.com. Their dedicated team is available to address concerns, provide information, and assist with appointments or consultations.
Final Words
Consultation with a vascular surgeon regarding vascular malformations is crucial because patients will undergo a comprehensive evaluation of the condition and personalised treatment planning. Vascular surgeons have specialised knowledge in the management of these complex conditions and can provide insightful information regarding available treatment options, potential risks, and anticipated outcomes. By consulting with a vascular surgeon, patients gain access to a comprehensive evaluation of their condition, individualised treatment plans, and a source of optimism, knowing that professionals are committed to enhancing their health and well-being.
Frequently Asked Questions:
Vascular malformations are rare developmental abnormalities involving blood vessels (arteries, veins, and lymphatics) that can occur anywhere in the body. They can manifest as soft tissue masses, pain, swelling, or skin discoloration and may require treatment for pain, functional impairment, bleeding, or other complications. These malformations disrupt normal blood flow as the vessels enlarge, tangle, or form abnormal connections. While they are typically present at birth, they can also develop in adulthood. Some types are extremely rare, affecting less than 1 percent of the population, and their symptoms may be triggered by factors like adolescence, pregnancy, surgery, trauma, or injury. Over time, vascular malformations can grow, invade surrounding tissues, and pose varying degrees of risk.
Arteriovenous malformations (AVMs) are abnormal growths of veins and arteries, lacking capillaries, and may affect the brain or spine causing pulsing sensations. Venous malformations (VMs) are enlargements of veins, appearing as bluish or skin-colored soft lumps under the skin, being the most common type of congenital vascular malformation. Lymphovenous malformations (LVMs) are non-cancerous fluid-filled masses that develop in soft tissues, often in the face, neck, or axillary regions. Dural arteriovenous fistulas form when fistulas arise between arteries and veins in the brain area. Haemangiomas are non-cancerous blood vessel growths, commonly seen as red birthmarks on infants, occurring anywhere on the body, particularly the face, scalp, back, or chest.
Surgical excision may require multiple sessions and can lead to recurrence or disfigurement if not fully removed. Minimally invasive methods, such as embolization and sclerotherapy, effectively halt the malformation’s growth, with some patients needing multiple sessions based on its size and type. Laser therapy addresses surface blood vessels and associated skin texture issues caused by haemangiomas, while interventional therapies offer alternatives for non-responsive cases or patients seeking non-pharmacological options.
It cannot be prevented. Vascular malformations are congenital conditions, and genetic counselling is advised for those with a family history to discuss risk reduction options. Early detection and proper medical care are essential for symptom and complication management. Support networks and advocacy groups offer valuable resources and emotional support for individuals and families impacted by vascular malformations.
A healthcare professional will evaluate the patient’s medical history and conduct clinical examinations and imaging tests to determine the malformation’s nature and extent. The treatment plan, which can include minimally invasive procedures, surgery, or other targeted therapies, will be discussed, with details about duration, potential risks, and adverse effects. The medical staff will prioritize patient comfort and safety by providing appropriate pain management methods. Following treatment, a recovery period will occur, with scheduled appointments for monitoring progress and addressing concerns or complications. Clear communication with the healthcare team is vital for understanding and managing expectations during treatment for vascular malformations.
References:
Cleveland Clinic. (2022). Vascular Malformations. Retrieved from
https://my.clevelandclinic.org/health/diseases/23409-vascular-malformations
Johns Hopkins Medicine. (2022). Vascular Malformations. Retrieved from
https://www.hopkinsmedicine.org/health/conditions-and-diseases/vascular-malformations
Mayo Clinic. (2022). Brain AVM (arteriovenous malformation). Retrieved from
https://www.mayoclinic.org/diseases-conditions/brain-avm/diagnosis-treatment/drc-20350265
SingHealth. (n.d) Sclerotherapy for Vascular Malformations. Retrieved from
Yale Medicine. (2022). Vascular Malformations. Retrieved from https://www.yalemedicine.org/conditions/vascular-malformations

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
- Tags:
- vascular malformation
