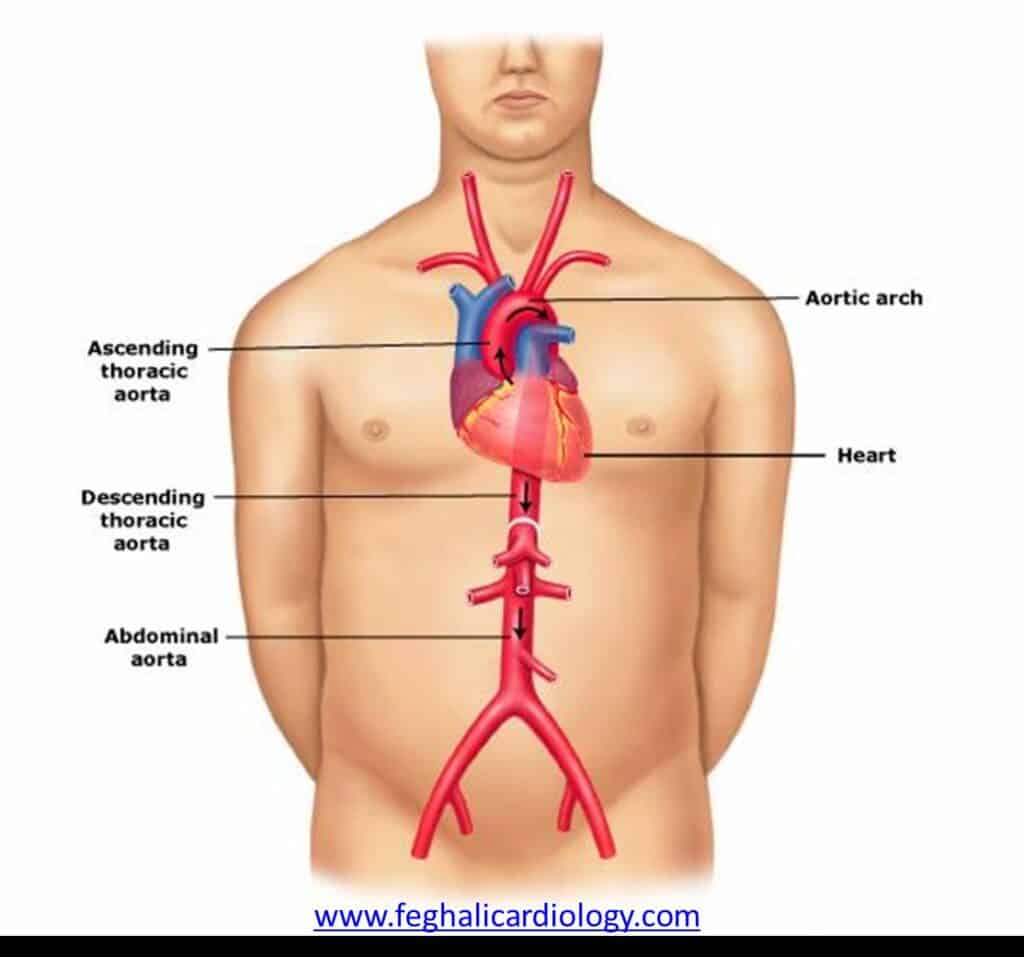
The Purpose of the Aorta
The aorta, a large vessel that begins from the heart and courses through the chest and abdomen, is the principal artery responsible for carrying oxygen-rich blood from the heart to the body’s various organs. As it travels, smaller blood vessels branch off to supply different tissues. Weakening of the aortic walls can lead to bulging, and when this occurs in the abdominal section, it results in an abdominal aortic aneurysm, a potentially dangerous dilation of the artery that requires medical attention to prevent complications.
(http://www.gadacanada.ca/aorta-taad)
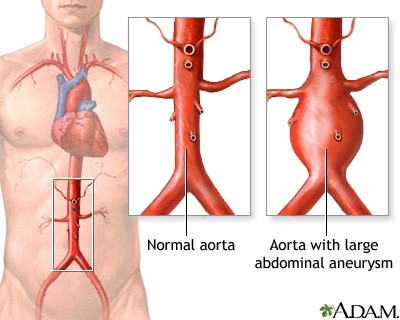
An Overview of the Aortic Aneurysm
An aneurysm develops when the walls of an artery lose strength, permitting pressure from within the artery to accumulate and result in the protrusion of a weakened segment of the artery wall. This outward bulge is recognized as an aneurysm. Specifically, an abdominal aortic aneurysm (AAA) denotes a dilation in the main blood vessel, the aorta, responsible for transporting blood from the heart to the body. This artery courses through the torso, supplying blood to vital organs like the liver and kidneys before dividing into two branches to extend down to the legs. Aneurysms carry the risk of rupturing, potentially causing severe internal bleeding that can swiftly become life-threatening.
(https://medlineplus.gov/ency/article/000162.htm)
Complications of Aortic Aneurysm
Aortic aneurysms present potentially severe complications that necessitate medical intervention. If an aortic aneurysm ruptures, it triggers internal bleeding, the consequences of which vary depending on the aneurysm’s location, often posing significant danger and even a threat to life. Swift medical intervention can facilitate recovery from a ruptured aneurysm for some individuals. Unfortunately, for most patients who experience a ruptured abdominal aortic aneurysm, massive life-threatening blood-loss occurs within a span of a few minutes even before medical help can arrive. The ideal time to treat an aortic aneurysm is before any symptoms develop and before it has ruptured.
The Three Types of Aortic Aneurysms
There are three primary types of aortic aneurysms based on their location within the body. The first type is known as a Thoracic Aortic Aneurysm (TAA) and occurs within the chest area. The second type is an Abdominal Aortic Aneurysm (AAA), which develops in the abdomen. The third type, called a Thoracoabdominal Aortic Aneurysm (TAAA), is situated between the chest and abdomen. These distinct types of aortic aneurysms have varying implications for diagnosis, treatment, and management.
During the initial phases, when an aneurysm (AA) is still small, it’s not an immediate threat to health. However, as the aneurysm keeps getting larger, it can lead to thinning of the aorta’s walls or the branches that come off it. This thinning makes them less capable of stretching and accommodating blood flow. The weakened parts of the wall might eventually become too fragile to withstand the force and pressure from the blood circulating through them. This situation could result in the aneurysm rupturing, which in turn could lead to serious internal bleeding and death.
Key Risk Factors for Aortic Aneurysms
These factors increase the likelihood of developing an aortic aneurysm:
- People who smoke regularly.
- Men over 65 years of age.
- Individuals with high blood pressure or heart problems.
- People with conditions like Marfan’s syndrome, Ehlers-Danlos syndrome, and Loeys-Dietz syndrome, which affect the body’s connective tissues.
- Having a strong family history of aortic aneurysms or dissections.
Symptoms of an Aortic Aneurysm
Aortic aneurysms can manifest with a variety of symptoms that indicate potential health concerns. These include persistent and severe pain experienced in the chest, abdomen, and back, or even extending down to the lower limbs. In some cases, individuals might experience a continuous fever that doesn’t subside. One notable sign can be the presence of a pulsating or throbbing mass felt in the abdominal area. Additionally, there might be unusual patches of gangrene developing in the toes, which could be a consequence of compromised blood flow. However most aneurysms are best treated before any symptoms occur and individuals with any of the above risk factors should go for screening to detect any presence of an aneurysm.
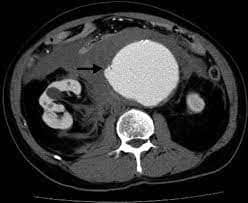
Diagnostic Procedures for Aortic Aneurysm
Diagnosis relies on a clinical assessment where an aneurysm might be palpated as a pulsating mass within the abdomen. To confirm the presence of an aneurysm, medical practitioners often advise undergoing an ultrasound or CT scan. Ultrasound uses high-frequency sound waves reflected off internal structures to generate real-time images. CT scans utilize X-rays taken from multiple angles to create cross-sectional images, which, when stacked together, provide a 3D view of the body’s internal organs and structures. Both imaging techniques play a vital role in diagnosing and monitoring medical conditions.
(https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.110.972018)
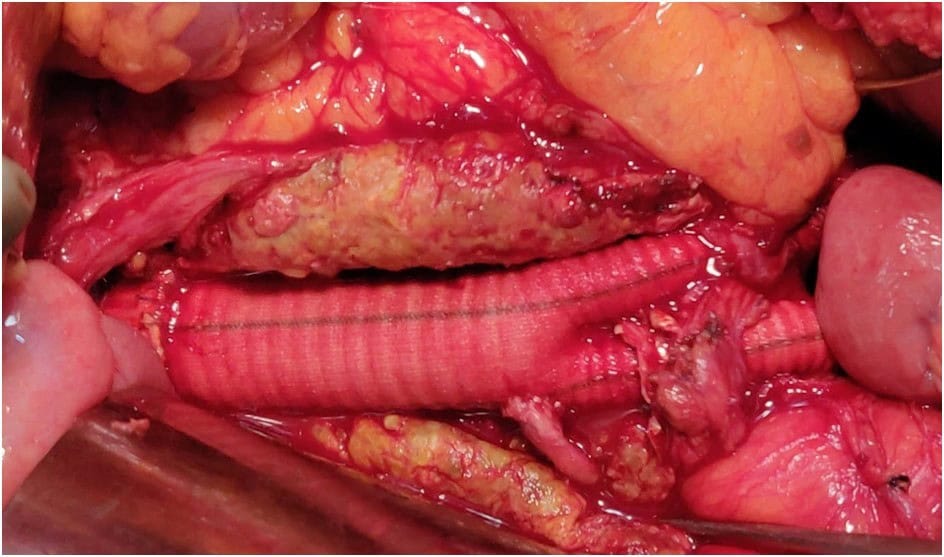
Traditional Treatment for Aortic Aneurysm: Open Surgical Repair
Open Surgical Repair is a traditional approach for aneurysm treatment, involving extensive chest/abdominal wall incisions. It’s considered effective but it carries higher risks due to its invasiveness, making it suitable mainly for younger individuals with low surgical risk. Recovery often involves around 1 week of ICU care and takes roughly 4 to 6 weeks for full recuperation.
(https://www.kauveryhospital.com/ima-journal/ima-journal-november-2022/abdominal-aortic-aneurysm/)
Minimally Invasive Treatments for Aortic Aneurysm
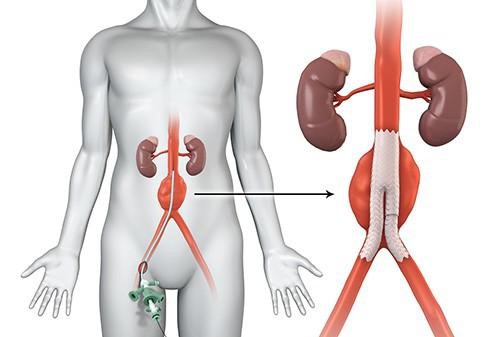
Minimally Invasive Repair, known as EndoVascular Aortic Repair (EVAR), involves using covered stent-grafts inserted through small groin incisions to treat aneurysms. The stents are placed in the affected area to redirect blood flow, guided by X-rays. EVAR is suitable for older patients or those with multiple health issues and offers the advantage of local anesthesia and mild sedation. Recovery is faster, often without ICU stay; patients are mobile within 8 hours and typically discharged within 48 hours. In certain cases, young and healthy patients may even be released on the same day as the procedure.
(https://radiology.wales/evar/)
Post-Treatment Recovery and Lifestyle Considerations
After aneurysm treatment, ongoing lifelong follow-ups are essential due to the potential for disease progression in other parts of the aorta previously unaffected. Development of thoracic aneurysms following abdominal aneurysms and vice versa is not uncommon, especially if risk factors like smoking and hypertension persist. Follow-up involves regular ultrasound and CT scans, initially every 6 months and later annually. This monitoring is crucial, particularly for patients who have undergone EVAR, as scans help identify potential leaks around the stent graft.
Reducing Your Risk of Developing Aortic Aneurysm
Preventing AAA (Abdominal Aortic Aneurysm) can be a complex challenge, especially when a family history of the condition is involved. However, taking swift action to consult a vascular surgeon is pivotal. This proactive approach to early detection and appropriate treatment holds the promise of restraining the aneurysm’s progression and rupture. Moreover, a range of risk factors can be effectively managed through deliberate steps:
- Quitting smoking
- Engaging in regular physical activity and maintaining a balanced, wholesome diet.
- Monitoring and regulating weight, blood pressure, and cholesterol levels.
- Exercising moderation in alcohol consumption.
FAQ
A vascular surgeon can assist in treating an aortic aneurysm by providing specialized care and interventions. They can monitor the aneurysm’s progression and recommend suitable treatment options based on the patient’s condition and lifestyle. The goal is to prevent aneurysm rupture, which could lead to life-threatening internal bleeding.
An aortic aneurysm is a medical condition where a weakened area of the aortic wall becomes dilated or ballooned, causing the blood vessel to expand beyond its normal size. This can lead to dangerous consequences, as the stretched and weakened wall becomes more susceptible to rupture, potentially resulting in severe internal bleeding.
Symptoms of an aortic aneurysm include severe and enduring pain in the chest, abdomen, back, or lower limbs, persistent fever, pulsating sensation in the abdomen, and reduced blood flow leading to potential tissue damage or gangrene in the toes. All these symptoms may indicate potential complications with the aneurysm, thus for better outcomes, treatment should sought even before such symptoms begin to manifest.
Aortic aneurysms are diagnosed through clinical examination, and imaging tests like ultrasound scans or CT scans, with incidental discovery during checkups, enabling accurate assessment of the aneurysm’s characteristics and size.
Traditional Surgical Repair involves Open Surgical Repair, a conventional approach for treating aortic aneurysms through chest/abdominal wall incisions to access and repair the aneurysm, but its invasiveness brings substantial risks and a longer recovery period. Minimally Invasive Repair, on the other hand, offers a modern alternative using EndoVascular Aortic Repair (EVAR), a less invasive procedure utilizing special stents inserted through small incisions in the groin to exclude the aneurysm from blood pressure circulation under X-ray guidance.
References
[1] https://my.clevelandclinic.org/health/diseases/7153-abdominal-aortic-aneurysm
[2] https://www.sgvascularctr.com/service/aortic-aneurysm/

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
- Tags:
- Aortic aneurysm
