Singapore Vascular and Interventional Centre
Why you might need fibroids treatment, Singapore.
WHAT ARE UTERINE FIBROIDS?
Uterine fibroids are a common condition among women. It occurs when benign or non-cancerous tumours develop in the uterus. In fact, by the age of 35, 40-50% of women have had uterine fibroids at some point in their lives. If that is you, we, the Vascular and Interventional Centre, are here for you! There is nothing to worry about as there are effective and established methods for treating and removing these uterine fibroids. Also, these growths are very rarely cancerous, with only one in 350 people having uterine fibroids that transform into a malignant or cancerous tumors.[8] The risk is therefore low and your condition can usually be treated easily with uterine fibroid embolisation (UFE, Singapore).
More specifically, uterine fibroids are excess growths from the myometrium, which is the muscular tissue of the uterus. Most of the time, the growth of uterine fibroids is stimulated by the female hormone oestrogen. There are many different variations to the way uterine fibroids can appear, either as a single fibroid or as a cluster consisting of multiple fibroids. As such, the size, location and number of fibroids in your uterus is never fixed,[2] so treatment options have to be considered on a case to case basis, tailored to your situation and symptoms. There are a few common symptoms that you could be aware of, as indicators that you may have uterine fibroids. For example, excessive and painful bleeding during menstruation (menorrhagia), lower back pain, bloating, constipation, and frequent urination.
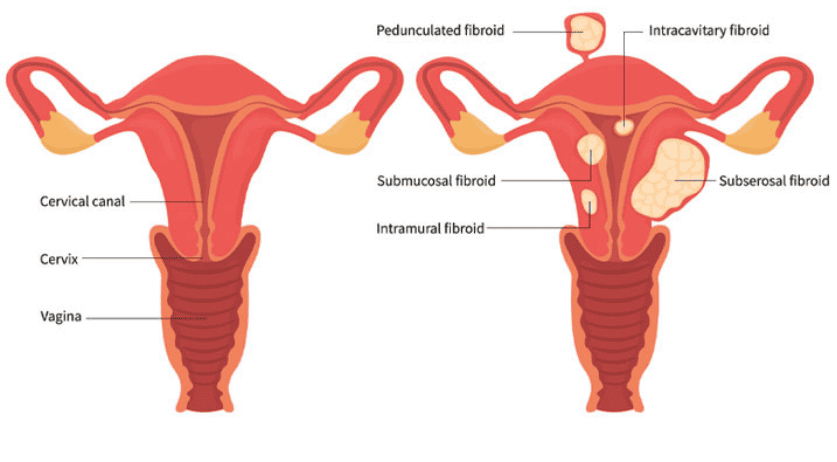
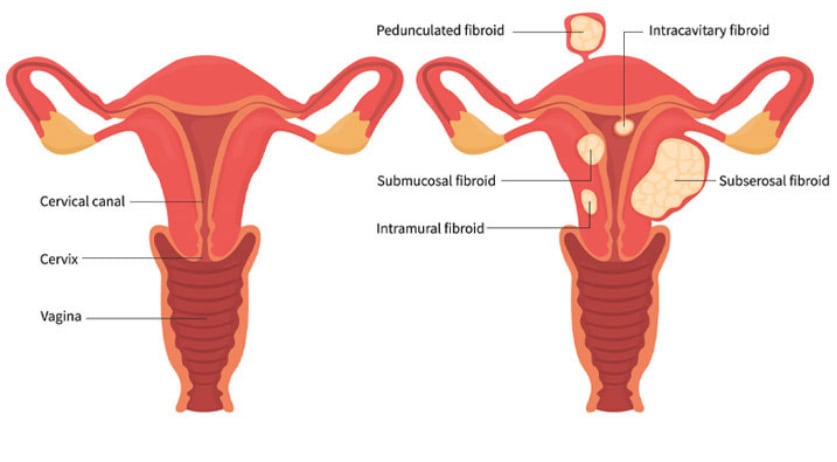
TYPES OF UTERINE FIBROIDS
There are 5 main types of uterine fibroids, namely intracavity, intramural, pedunculated, submucosal and subserosal, as seen in the image below.[5] Depending on their location and type, fibroids can cause different symptoms.
[7]
- Intracavitary fibroids: these uterine fibroids have grown almost completely into the uterine cavity. Because of their position, intracavitary uterine fibroids tend to be associated with infertility, by physically blocking sperm as it travels to the fallopian tubes.
- Intramural fibroids: these uterine fibroids are found within the walls of the uterus. This type of uterine fibroids is the most harmless to your body. Because they do not act as physical barriers for fertilisation or implantation within the uterine cavity, their effect on fertility is quite minimal. However, like all uterine fibroids, they require a blood supply to keep growing, and hence the circulation of blood around the uterus is affected to sustain the growth of these uterine fibroids. This blood supply is taken from the uterine artery, which could mean that other organs supplied by the uterine artery may receive less blood. The endometrium (wall of the uterus) itself would also be less vascularised, which means fewer blood vessels would be supplying it with blood, and this could potentially affect the uterus’ ability to support a healthy pregnancy.
- Pedunculated fibroids: these uterine fibroids are either found in the uterus or outside of the uterus, attached to the uterine tissue by an elongated stalk. If these uterine fibroids are twisted because of any sudden movements you make, severe pain may be experienced.[6]
- Submucosal fibroids: these uterine fibroids grow partially into the uterine cavity from the walls of the uterus. They lie right under the lining of the uterine cavity. They can cause infertility in women in the same way that intracavitary uterine fibroids do.
- Subserosal fibroids: these are uterine fibroids that grow partially out of the uterus from the walls of the uterus, and are the most common type of uterine fibroids. These have a lesser effect on fertility, but they can cause some discomfort by placing pressure on your nerves around the area. Sometimes, they develop and stalk and become pedunculated uterine fibroids.
DIAGNOSIS OF UTERINE FIBROIDS
In order to determine whether you have uterine fibroids or not, ultrasound scans and MRIs can be used to accurately diagnose. [1]
Ultrasound scans involve soundwaves as an imaging technique to better visualise the position of uterine fibroids in your uterus.[3] A gel is first applied to your abdominal area to minimise the air spaces between the transducer (scanner) and your skin, such that a clearer image can be obtained at the end of the scan.[4] This is needed as ultrasound does not travel very well through the air, and without the gel, the final images would not be clear. This is a simple procedure that should take around 20 to 30 minutes. Alternatively, a transvaginal ultrasound may also be conducted.
MRI scans are radiation-free and involve the use of magnetic waves to visualise the pelvis and uterus. Results are more detailed than that of ultrasound scans and also involve the use of larger equipment. This procedure is completely safe and harmless, so you should not experience any discomfort at all.[6]
Your doctor will advise you on the most suitable method of diagnosis for you, such that there is minimal risk posed to your health. Always remember to consult a medical professional for confirmation of your personal health situation, and avoid self-diagnosis. Although your quality of life may not be affected by the presence of certain types of uterine fibroids, you should get them assessed regularly such that the doctor can keep track of whether the uterine fibroids are growing larger. Treatment is recommended if you start displaying symptoms and have discomfort that affects your daily activities. As mentioned earlier, fibroids treatment, Singapore, usually refers to Uterine Fibroid Embolisation (UFE, Singapore).
Symptoms of Uterine Fibroids
The term “uterine fibroids” traditionally denotes benign tumors of the muscular coat, which comprise 99% of all pathological neoplasms in the muscle of the uterus. Clinical manifestations depend mostly on the size, location, and number of fibroids within the uterus and thus vary widely between patients. Fibroid size shows an asymmetrical distribution, varying from as small as 1-2 mm to as large as 35 cm in diameter. The most common symptoms that usually bring a woman to the doctor are the following: Heavy blood loss during menstruation is the most common complaint, with 25-49% of the patients nineteen years of age or older complaining about it. Fibroids exacerbate symptoms already present. Pain and discomfort are also quite common. In 29.4-55% of females, it is severe enough to result in missing days of work or class. In addition to daily activities, fibroids have been shown to impair a person’s sleep. Pelvic discomfort is more common among women who are at least 25 years of age. The greater the size of the fibroids, the more problematic the pressure they exert on the surrounding organs. Many women experience a variety of symptoms concurrent with the ones listed, while others may not experience any due to the heterogeneity of fibroids. Hence, if many women with fibroids do not display any symptoms, some people can undergo unnecessary surgery. Just as the signs and symptoms are not universal, managing fibroids is not about a one-size-fits-all therapy. Rather, the course of action is tailored to the individual needs, values, and health conditions of the patient.
Overview of Common Symptoms
A significant number of women report having no symptoms associated with the presence of uterine fibroids. Nevertheless, many women who have fibroids also experience symptoms. Such symptoms can vary greatly in terms of type and intensity. Common physical symptoms include excessive menstrual bleeding and/or the presence of clots, pelvic pressure or pain, frequent urination that may not be a urinary tract infection, and feelings of fullness or swelling of the lower abdomen. Many women with fibroids notice an increase in their abdominal size; some describe a sensation of fullness or swelling, or even a feeling that they are pregnant. Lastly, because there is sometimes an aesthetic and functional deformity of the abdominal wall associated with fibroids, women who have them may feel more embarrassed about their body’s appearance. Those with multiple large fibroids that alter the symmetry and balance of the abdomen might even look bloated. Involvement of surrounding organs like the colon can even lead to mild digestive problems.
There are many emotional and psychological symptoms related to having fibroids as well, which have received increasingly more attention. After all, a woman’s overall health reflects her mental and spiritual well-being as well. Women with fibroids can be diagnosed with anemia; they often must plan their life around their menstrual bleeding, may be shamed by their sexual partners because of heavy menstrual bleeding during intercourse, or may feel generally irritable and depressed. Some women also report that their fibroids can interfere with the quality of sleep. All of these symptoms clearly indicate that fibroids have the potential for significant debilitating effects. It is important for patients to remember, however, that they are the best judges of what they feel, and they should not necessarily be influenced by what other women’s symptoms are, or by what symptoms are known to be most common.
Variability in Symptom Severity
The range and severity of symptoms women experience with fibroids vary widely. Some women have mild symptoms. Others have symptoms so debilitating that their daily activities are awkward, if not impossible. In general, the symptoms caused by fibroids depend on many factors, one of the most important of which is the size and location of the fibroid(s). The location also has a major influence on the kind of symptoms experienced – a submucous fibroid can lead to such heavy periods that a woman becomes unhealthily anemic and needs a blood transfusion. A very large fibroid pressing on the rectum can either make it difficult to pass feces or give rise to painful defecation (or both).
A woman’s symptoms can worsen dramatically or multiply over time, or she can remain virtually symptom-free. This variability in symptom severity has led some to predict that the same variety and quantity of fibroids will have different effects in different women. It is essential, therefore, that any treatment decision is tailored to the woman’s particular case and that decisions are continually reviewed at regular assessments. If fibroids have such widely diverse effects, should we be surprised if we find differences between the severity of the symptoms reported by individual women? Yet there is anecdotal evidence of misdiagnosis, under-treatment, or being actively discouraged from treatment. In a situation of such complexity, it is difficult to adequately inform a woman even about her surgical treatment options if recovery time and return to normal activities is such a variably experienced risk. All we can do is to be aware of the range of individual experience. To acknowledge and explore the potential differences in clinical trial outcomes between different women, taking into consideration not only the size and location of fibroids but also differences in age, child-bearing desire, and other considerations.
Impact on Daily Life
Uterine fibroids can greatly impair a woman’s daily life. The excessive menstrual blood loss from a fibroid can lead to significant fatigue. Many women are unable to pursue and maintain demanding work schedules and social activities due to the embarrassing frequency and unpredictability of menstruation. In other cases, women have to take time off from work because of severe uterine fibroid symptoms. Menstrual blood loss can be so heavy that many women develop a profound knowledge of every public restroom in their area. Women with excessive menstrual bleeding are likely to suffer from pelvic pain and pressure. If they are sterile, they may attribute their infertility to their fibroids, which can lead to anxiety and/or depression.
The knowledge may also affect their expectations and decisions for expanding their family. Being sexually active with a significant other may be jeopardized by the unpredictability of such symptoms as irregular bleeding or pain. There may be variations of fibroid symptoms in different cultures, or hidden emotional issues that are not appropriate to share with strangers. These issues are all in need of a holistic approach, but for this approach to be considered, all possibilities must be explored. It is important for healthcare providers to acknowledge the practical issues for women living with symptomatic fibroids and initiate an honest, open discussion as part of the holistic approach.
Treatment Options
There are a wide variety of treatment options that are aimed at the relief and management of the signs and symptoms associated with uterine fibroids. The approach to the treatment of uterine fibroids is made on an individual basis that takes into account other factors such as the size, position, and number of fibroids a patient has, as well as her age, general health, and personal preferences. Women need appropriate information and education to make fully informed choices about their health care. Help and support may be accessed through support groups and expert multidisciplinary teams who are able to explore treatment options in depth.
Medication therapy is commonly considered in the management of uterine fibroids. Hormonal treatments offer relief from heavy menstrual bleeding by increasing the turnover of the lining of the womb. Pain management through the use of painkillers can be helpful for treating the discomfort experienced by women with fibroids. Uterine fibroid embolization is a procedure that is suitable for the treatment of large and medium sizes and numbers of fibroids. It is minimally invasive, not requiring open surgery, and involves blocking the blood vessels that go to the fibroids using small particles. This leads to degeneration of the fibroids, which offers relief from many of the symptoms associated with fibroids. Surgical treatments are generally considered in the treatment of uterine fibroids, and the most commonly offered surgeries of myomectomy and hysterectomy depend on a woman’s future reproductive and fertility needs.
Uterine Fibroid Embolisation (UFE)
Uterine fibroid embolisation is a non-surgical method for the management of uterine fibroids. It involves a detailed angiogram of the pelvis to identify both the uterine and ovarian arterial blood supply, followed by selective catheterisation and a further angiogram with saline to assess the arterial anatomy. Once the arteries supplying the fibroids have been identified, 500 mg to 1 g of small beads is slowly injected into the arteries. This is continued until there is sluggish or arrested flow in the arterial vessels. The beads can be exchanged with or followed by slow injection of more beads, in most cases, to ensure both the uterine and ovarian arteries are blocked. The injected beads lead to a decreased oxygen supply to the fibroids, resulting in a shrinkage of the fibroids. The procedure is completed on both sides, and the removal of the skin nick closure base is performed.
The UFE procedure is performed under a light general anaesthetic and takes around 1.5 to 2 hours to complete. Average hospital stay is typically 1 to 3 nights post-UFE, depending on patient factors. Air is injected from the groin, and the arteriole puncture is sealed by a combination of ice, pressure dressing, air, or needles. A waterproof dressing is used so the patient can shower, and all patients undergo an MRI at 3 months post-procedure to evaluate the success of the UFE. The MRIs are reviewed with a radiologist who details if the procedure has been successful, and a report is sent out to the patient outlining the same, if successful. If patients are symptomatic or signs indicate a more accurate evaluation, a delayed contrast-enhanced MRI can be performed. Patients are reviewed in an outpatient setting six months after the procedure has been performed, where a further MRI and an ultrasound are undertaken. At twelve months, a further MRI is performed. If there are new fibroids, he reviews patient symptoms.
Medication Therapies
Initiating medical therapy is the cornerstone of treating symptomatic fibroids. Several medication management options are available. Although medical therapy can treat fibroid symptoms, it does not change the size of the fibroids or make them go away. Consequently, if one decides to try these treatment options, her symptoms should be the primary motivation. A patient’s treatment plan should be personalized to address her individual concerns, the size, location, and rate of fibroid growth, her desire for future pregnancy, her medical condition, the importance of her symptoms, and the risk she is willing to undertake for medical therapy. Hormonal therapy, such as birth control pills or progestin-containing IUDs, can help control bleeding and assist non-fertility-oriented treatment plans by preventing irregular bleeding, iron-deficiency anemia, and the need for repeated iron infusion or frequent blood transfusion. Hormonal therapy does not make fibroids go away or decrease their size. Another option is taking non-hormonal pain relief medications. This is not a specific treatment for fibroids, but these medications can also help manage headaches, back pain, or cramps.
Other treatment options include taking medicine by mouth to manage heavy bleeding; these medications may or may not help this symptom. If the patient’s fibroids cause pressure-like symptoms in her pelvis, some medications might temporarily reduce the pressure. If a patient is trying to get pregnant or carry a pregnancy, neither of these options is suitable. Her healthcare provider can go into further detail and determine if such treatment is safe or acceptable in the unique context of her health and pregnancy status. Medications can result in several side effects. After treatment is begun, the patient should keep in close contact with her healthcare provider to make sure she is healing, especially if she is new to the medication. Also, if the patient does not feel that her symptoms are well controlled following therapy, her healthcare provider should explore additional opportunities. Additionally, medication is often not a permanent solution to fibroid problems, and symptoms will normally return. Patients and healthcare providers are encouraged to keep a discussion going so that everyone is aware of possible alternatives as the condition changes. Patients affected by fibroids are encouraged to find a healthcare provider with experience in dealing with fibroid problems.
Surgical Interventions
For various reasons, there are instances when women suffering from uterine fibroids would need to undergo a surgical intervention. One example would be because medical treatments have failed, are contraindicated, or are unsuitable. A second example would be if the size of the fibroids is such that they are pressing onto the bladder and/or bowel, affecting normal function. Unlike the interventions discussed in the previous section that contemplate aggressive fertility treatments, the intention for a surgical intervention is not to increase fertility rates but to treat the fibroids themselves.
Surgery that aims to remove a fibroid while conserving the uterus is termed a myomectomy. This option would be the surgery of choice for women who wish to maintain their fertility and preserve their uterus, depending on the size and location of the fibroids. A hysterectomy is a surgical procedure to remove the uterus itself and may be more suitable for women who have completed childbearing, although this is more commonly performed in the presence of complications such as very heavy and unpredictable periods, anemia requiring blood transfusion, persistent pain that is not being helped with analgesia, or the presence of a prolapsed uterus. The effectiveness and risks of each of these options will be discussed in this section in order to assist women in their decision-making. The process of discussing these options with surgeons and healthcare providers has been noted to help increase satisfaction arising from the final decision reached.
Although this guide focuses mainly on a multidisciplinary gynecological approach to fibroids and their management, many of the surgical interventions recommended for the treatment of fibroids will require the expertise of a surgeon. It is important to be aware of all potential treatment options available to any one woman and what can be offered by various healthcare providers. Surgeons capable of performing various types of fibroid-related interventions may or may not work as part of a multidisciplinary team, and it should be noted that this is not necessarily a measure of their standard of care. A range of treatments will be discussed in this section, and the reader, with their healthcare provider, should make a decision based on the best treatment options available to them. The outcome of surgery, like all options in the treatment of fibroids, should be discussed in the context of the evidence base and a woman’s own uterine fibroid burden, symptomatology, any malignancy risk, and desire for future fertility.
Causes and Risk Factors
Hormonal influences are believed to play a role in the development of fibroids. There is evidence to suggest that estrogen and progesterone can increase the growth rate of myomas. Family history with uterine fibroids and heredity play a role in the development of fibroids. Women with a hereditary predisposition have a considerably higher likelihood of developing fibroids. Being overweight or obese may also increase the likelihood of developing fibroids. Evidence is mixed concerning whether some dietary components play a part in the development of fibroids. Lifestyle and dietary factors that can lower the risk of fibroids include physical activity, including vigorous activity, fruit, and an increased intake of nutrients that are associated with fiber. Evidence shows that women in their reproductive years are more likely to develop fibroids. Fibroids in postmenopausal women are less likely to grow. Moreover, African American women are at a higher risk for fibroids at a younger age compared to women of other ethnic groups. Although fibroids are common among women of African descent, there are only a few reports on the prevalence of fibroids in African females. Research indicates that fibroids are more common in African Americans than in other ethnic groups. Moreover, a woman’s reproductive history may increase the risk of developing fibroids. Evidence shows that early menarche may increase the risk of developing fibroids. The older a woman becomes, the less likely fibroids will grow. Having children usually reduces the growth of fibroids, as childbearing helps reduce estrogen levels. Identifying risk factors for fibroids can aid in raising public awareness. Health care providers can help in reducing risks by providing preventive strategies in education and patient assessments.
Potential Causes of Uterine Fibroids
Speculating about possible sources of predisposition for uterine fibroids in some women, observations around several possible causes have been based on existing literature or derived from the results of other diseases. The hypotheses about the etiopathogenesis of leiomyomata are, in turn, set into several categories, including hormonal factors, growth factors, and scarring models. This section investigates the possible etiopathogenesis of leiomyomata in the aspect of hormonal regulation and indicates a potential change in the approach to the treatment and management of this highly prevalent disease. Hormonal factors are one potential cause that has been speculated to be a factor in predisposition to uterine fibroid development. It is known that the predisposition for developing leiomyomata in women is related to estrogen and progesterone throughout their lives, being most common in women of reproductive age and usually regressing or becoming pregnant. Estrogen, whose main source is an ovulatory ovarian follicle, has a stimulating effect on myoma cells. On the other hand, it inhibits progesterone-induced apoptosis and promotes collagen production, making the muscle cells of the middle layer contract. The role of progesterone is even more gradual, inhibiting the conversion of active androstenedione to active estradiol, causing endometrial erosion or necrosis via the metalloproteinase matrix, promoting inflammation and stimulating the secretion of chemotactic fibroblast growth factor for myoma cells. Possible causes, besides hormonal, that may contribute to uterine fibroids are also genetic ones. It also cannot be ruled out whether the reason for the growing prevalence of fibroids is the result of increasing awareness and reporting of the disease rather than being purely biological. An important exposure is also environmental and lifestyle factors, such as sports and physical activity, high consumption of green vegetables and fruit, fat, alcohol, and caffeine. Some others emphasize the need for further scientific research.
Identifying Risk Factors
Knowing the risk factors that have been linked to fibroids is central in understanding the condition and the process of fibroid development. These risk factors identify women who are more prone to develop fibroids. Factors that have been associated with fibroids include age, ethnic background, reproductive history, family history, obesity, and possibly diet and lifestyle. Knowing how these risk factors are linked to fibroids can help develop new ways of treating women with fibroids according to their own risk profile. Age: Fibroids are more prevalent in women in their 30s and 40s. While it is rare in teenagers younger than 15 years of age, around 2 to 3 per 10 women develop fibroids by age 50. Fibroids are least frequent in those under 30. The incidence of fibroids decreases with further increase in age beyond 50 in women. Ethnic background: Fibroids are more frequent in Black women than White women. Additionally, other studies have shown that they are also equally common in Afro-Caribbean populations and are least frequent in the White population. Reproductive history: Early menstruation, giving birth to at least one child or two children, and late onset of menopause are some of the factors that have been linked to a higher risk of fibroids. Other risk factors include regular episodes of pelvic pain or prolonged menstrual flow. Women should reflect upon these risk factors and then consult their GP formally if these increase the clinical suspicion for fibroids in individuals.
Prevention and Management
Lifestyle changes could potentially prevent the onset of uterine fibroids and manage symptoms when they begin to show. The key is to support hormonal balance and take care of reproductive and sexual health. A balanced, healthy diet full of fruits and vegetables and regular moderate exercise can be helpful. If you are unhappy with your diet or are not sure if it is benefiting your hormones and especially fibroids, a dietary consultation can offer broader insights. The same goes for exercise and other lifestyle and stress management factors. A dedicated nutritionist can work with you to tailor a healthy diet plan that supports healthier hormone balance and also manages any other health conditions you may have. Be aware of any unusual pains or bleeding between periods to ensure any reproductive health problem that develops is detected early. Regular health check-ups are very important. It is also crucial to understand how stress impacts hormonal health and may contribute to fibroid growth. Strategies to prevent fibroids, or any other reproductive health issue, should focus on balancing key hormones. Be proactive about your own health and work with health professionals to find the best solutions. Start now by making an appointment with a primary care or women’s health doctor. If you are already having periods, it can be helpful to learn about menstrual health and healthy menstruation, so you can easily identify if you develop any symptoms of unusual period pain or other issues that do not feel right. Minimize stress. This can be very important because fibroids are very sensitive to the hormone cortisol. Practicing mindfulness and relaxation techniques can be very helpful. Whether it’s yoga, walking in nature, getting massages, or just spending time with family and friends, learning how to relax can make a difference. A stress-relieving activity for one person may not be the same for another. Try different ways of relaxing and find what works best for you. Learn about stress management techniques and tools within days. Regular exercise can have a positive effect on reducing stress levels. Some exercise programs also recommend gentle stretching or yoga movements, and these activities can be helpful. Ensure you are consuming enough energy and nutrients after regular moderate exercise. Nutritional supplements and balancing nutrient deficiencies with diagnosis are common. Nutritional supplements are not a substitute for a balanced diet. Avoid intense exercise that can cause over-exercise. Calorie restriction without adequate energy can disrupt hormone balance. Regular exercise, reducing obesity with a balanced diet, and long-term strategies for managing weight are usually recommended to improve health over time.
Lifestyle Changes
There is no evidence that diet alone can directly prevent or treat uterine fibroids. However, a nutritious, balanced diet can be wise. Foods high in added sugars, processed ingredients, unhealthy fats, and high sodium should be eaten minimally. A healthy diet is packed with greens, such as fruits and vegetables, lean proteins, and whole grains.
Regular physical activity can help overall health and wellness. It can also help to control weight. Since uterine fibroids are sensitive to estrogen levels, weight can be a contributing factor in fibroid growth.
Overall Well-Being and Stress Management Self-care activities are also integral to hormonal balance and overall well-being. Managing stress levels is crucial, as increased stress can lead to imbalanced hormones. Stress can also decrease the body’s immune system functioning. Strategies for emotional well-being may also aid in preventing and managing uterine fibroids.
Sleep Adequate and consistent sleep is crucial for overall reproductive health and for maintaining hormonal balance.
Finding healthy outlets and coping mechanisms for stress can also be beneficial in preventing and managing uterine fibroids. Engaging in activities that you find relaxing or that bring you joy is important. Regular self-care is pivotal to living a physically healthy life. The lifestyle changes listed above impact general health and wellness. Those diagnosed with uterine fibroids can also include recommended self-care for fibroids as an additional tip. Taking a comprehensive approach to living well overall is generally a good idea. No one can predict the future, and making choices that support overall health is wise, as is seeking care and screenings regularly.
Preventative Measures
Finally, a few measures to take in order to prevent uterine fibroids from developing include the following recommendations. If various imaging options are available, then regularly screen for any existing uterine fibroids. In cases of abnormal and/or very heavy menstrual bleeding, or if any abdominal growths are noticed or felt, seek an immediate consultation with a healthcare provider. Such screenings can also be a part of regular reproductive health visits with a healthcare provider for prevention and overall wellness. Women and girls should be aware of their personal and family medical histories, including relatives experiencing any irregular or heavy menstrual bleeding. This awareness of one’s family history can contribute to a more comprehensive risk assessment. Family members can be advised to also seek regular screenings during their discussions about health conditions that may potentially be hereditary, such as high blood pressure, diabetes, and certain types of cancer. A healthcare provider can work with a woman on her history and personalized risk level in addition to an ultrasound that can help show existing fibroids. Though no singular known preventive measure could guarantee against getting uterine fibroids, general lifestyle modifications such as changing dietary habits, doing moderate exercise, and re-learning some stress management techniques could maintain and even foster reproductive health in both women and men. Various imaging options are available to regularly screen for any existing fibroids and whether any fibroids have likely already grown within the uterus. Healthcare providers often recommend non-enhanced ultrasound screenings. Screening can often be sought at multidisciplinary healthcare facilities and gender departments within an organization.
If you have been diagnosed and would like to receive treatment for uterine fibroids, Singapore Vascular and Interventional Centre is here for you. Feel free to book an appointment with our doctors, Dr Benjamin Chua and Dr Manish Taneja.
Contact us with the details below:
+65 6694 6270 (Call)
+65 9898 3595 (WhatsApp)
en*****@sg***********.com (Email)
Novena Specialist Centre #06-08, 16-19
8 Sinaran Drive, Singapore 307470
REFERENCES
[1]https://www.nuh.com.sg/Health-Information/Diseases-Conditions/Pages/Uterine-Fibroids.aspx
[2]https://my.clevelandclinic.org/health/diseases/9130-uterine-fibroids
[3]https://www.mayoclinic.org/diseases-conditions/uterine-fibroids/diagnosis-treatment/drc-20354294
[4]https://ecovue.com/news/what-ultrasound-gel-does-to-your-patients-skin/
[5]https://www.gleneagles.com.sg/specialties/medical-specialties/women-gynaecology/uterine-fibroid
[6]https://www.nhs.uk/conditions/mri-scan/
[7] https://www.gleneagles.com.sg/specialties/medical-specialties/women-gynaecology/uterine-fibroid
8 https://my.clevelandclinic.org/health/diseases/9130-uterine-fibroids
- Tags:
- Fibroid
- Fibroids
- Uterine Fibroids
