Introduction to DVT
Deep vein thrombosis (DVT) is a blood clot that forms inside a deep vein within the body, usually in the legs and less commonly in the arms. A clot can form for various reasons, such as damage caused by surgery or injury, sitting down for long periods of time, or increased inherent clotting tendency due to pregnancy or genetics.
Causes, Symptoms, and Risk Factors of DVT
DVT is caused by a triad of factors, namely poor blood flow (venous stasis), increased clotting tendency (hypercoagulable states), and injury to the vessel wall (endothelial damage).
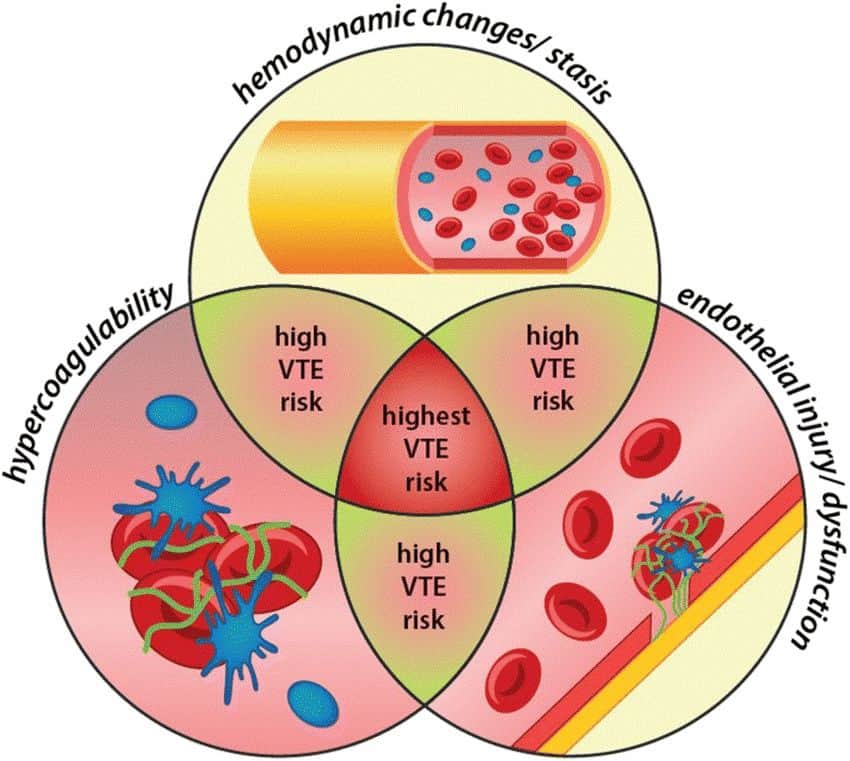
(Image source: https://www.researchgate.net/publication/330883723_Impact_of_drugs_on_venous_thromboembolism_risk_in_surgical_patients/figures?lo=1)
Causes of poor blood flow include obesity and pregnancy, where the increased pelvic pressure obstructs the veins making it harder for blood from the legs to flow back to the heart. Prolonged periods of immobility (such as prolonged bed rest after a major surgery or sitting for hours during a long-haul flight) also leads to poor blood flow in the leg veins. The leg veins are thin-walled low-pressure vessels, and they rely on the surrounding leg muscle contractions to push the blood back to the heart. During periods of prolonged immobility, blood is unable to move by itself upwards and begin pooling in the deep veins of the leg thus leading to DVT.
Increased clotting tendencies also occur in pregnancy but can be a result of genetics and cancer as well. It is especially so, if you experience recurrent DVTs, without any obvious inciting factor. External factors such as birth control pills, hormone replacement medications and smoking can also increase the risk of forming clots in the deep veins.
Injury to the vein, leading to a DVT usually occurs after trauma such as from a motor vehicle accident, or from surgery. The deep vein may also be injured from recurrent external compression by surrounding structures such as in thoracic outlet syndrome or popliteal entrapment syndrome.
The most common symptoms suggestive of a DVT include sudden pain in your leg or arm (which can worsen when standing or walking), swelling in the affected area(s), and/or skin discoloration.
Diagnosis of DVT If you believe you may be suffering from a deep vein thrombosis, it’s essential to seek medical help immediately. Your doctor will likely conduct an ultrasound of your affected veins and a Doppler test, which evaluates how blood flows thru the vein. Additionally, they might take a blood test or ask for CT scans to evaluate the veins within the chest and abdomen for any evidence of clots.

(Image source: https://4dbabyscanslondon.com/dvt-screening/)
Medications and Treatments for DVT
The treatment options for those who suffer from DVTs will depend on many factors such as age, general health, severity, and location of the clot(s). Outlined below are some of the treatment options available:
1. Blood Thinners
These medications are typically prescribed to help stop any further formation of clots and break up existing ones within an individual’s veins and arteries. This helps reduce associated risks like pulmonary embolism, which occurs when part of the clot breaks away from the main source and travels to a person’s lungs.
2. Minimally Invasive Treatments
In some instances, surgical intervention may be necessary and this can involve either infusing medications into the vein via a long tube/catheter to break up the clot (such as in thrombolysis), or by mechanically removing the clot itself (thrombectomy) by using specialised devices which are introduced via a small puncture wound.
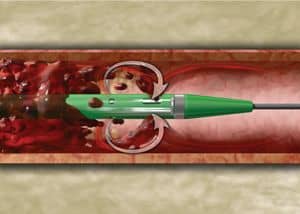
(Image source: https://www.bostonscientific.com/en-US/products/thrombectomy-systems/angiojet-thrombectomy-system.html)
3. Compression stockings
Compression stockings are used in the prevention of DVTs. These are garments that apply pressure around the legs and calves to reduce the polling of blood in the corresponding veins, thus reducing the risk of DVT forming.

(Image source: https://www.amazon.in/Compression-Stockings-Thigh-Unisex-Moderate/dp/B093CH124L)
Prevention of DVT
Prevention is always the best way to tackle any medical problem, and should be practised by all, but especially by those who have known risk factors. One way to do this is by maintaining a healthy and balanced lifestyle — exercising regularly, eating nutritious foods, and avoiding smoking if possible. Additionally, those more prone to blood clots should consider wearing compression stockings and even taking anticoagulation medications under supervision of a doctor, when traveling on long trips.
Complications of DVT
DVT if left untreated may progress and lead to severe consequences such as:
- Limb loss – the circulation of the affected arm/leg progressively deteriorates leading to irreversible tissue damage and an unsalvageable limb.
- Pulmonary embolism – this is a condition whereby a segment of the clot breaks away and lodges in the main vessels of the lungs (pulmonary artery) leading to a lack of oxygen, which can be life-threatening.
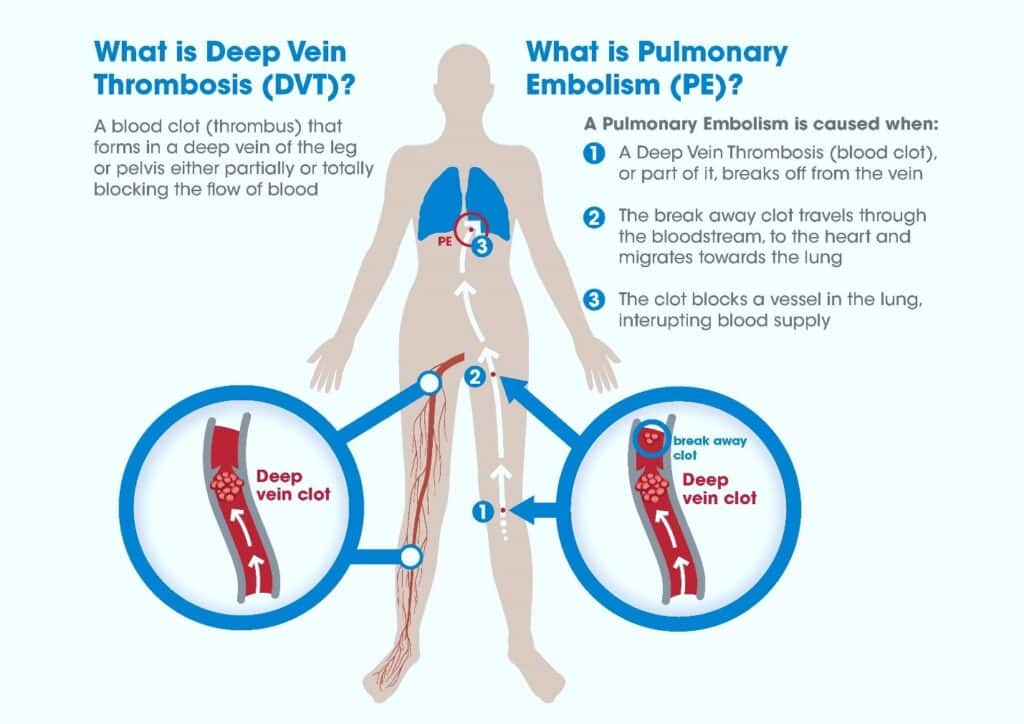
(Image source: https://www.capital-medical.com/products/dvt-pe-treatment/)
3. Post-thrombotic syndrome – the clot in the vein leads to inflammation and over-time damage to the valves. This results in long-term malfunctioning of the deep veins leading to persistent leg swelling.

(Image source: https://www.nhs.uk/conditions/deep-vein-thrombosis-dvt/)
Recovery from DVT
The best way to recover from a deep vein thrombosis event is to follow medical advice as closely as possible; this means taking all prescribed medications, wearing compression stockings if needed, and returning to a regular exercise routine when able to (as approved by your physician). It also helps if you maintain healthy habits like eating nutritious foods and avoiding smoking and alcohol consumption.
DVT and Lifestyle Considerations
1.Travel – For those considering taking long domestic or international trips, it’s vital to keep DVT prevention methods in mind. This means staying active while traveling (if possible) and elevating your legs to encourage proper circulation; flights over four hours should include a 15-minute break every so often if possible. Additionally, wearing compression stockings may be wise for those hoping to reduce their risk during travel. Taking plenty of fluids to avoid dehydration also helps.
2.Pregnancy – Expectant mothers have an increased chance of developing deep vein thrombosis due to slowed blood flow caused by the enlarging foetus as well as increased clotting tendency due to the pregnancy hormones. Pregnant women must take precautions to avoid any potential clotting issues, including regularly exercising or moving around, avoiding sitting positions with crossed legs, wearing compressing socks at night, and maintaining adequate hydration levels throughout the day.
3.Children – Children are typically not at the same risk as adults when developing clots, although certain conditions, such as birth defects or illnesses, may increase their chances. If your child shows any signs of DVT (such as leg or arm pain, discoloration, and general fatigue), you should take them to a doctor immediately to rule out any underlying issues.
When To See a Doctor For DVT
Seeking medical help is an absolute must if you suspect you or someone else is experiencing a profound vein thrombosis event. Not only will this help ensure proper testing to identify the clotting issue(s), but also that appropriate treatment options can be provided depending on the severity and location of clot formations — this could potentially save lives.
FAQs:
Yes. Traveling can be a major risk factor for DVT, so it’s important to take preventative measures. Staying hydrated and active on long trips is key; avoid sitting in one position for too long by getting up and walking around regularly throughout your journey. Wearing compression socks or stockings also helps improve circulation and reduce the risk of clots forming in your veins.
During pregnancy, you can decrease your chances of developing deep vein thrombosis by keeping as active as you can—regular walks or low-impact exercises are great options here! You should also stay well hydrated and sleep with your legs slightly elevated above heart level if possible (by placing pillows underneath them). It is also important to stay hydrated by drinking plenty of fluids.
Any signs of swelling or discoloration in your extremities should be investigated immediately, as they may be a sign of an underlying clot. The pain associated with DVT can range from moderate to severe depending on the degree of vessel obstruction and usually gets worse when walking or standing up. If you notice any of these symptoms, then it’s important that you seek medical assistance right away so that treatment can begin before it’s too late.
Common side effects associated with using blood thinners for Deep Vein Thrombosis (DVT) include nausea, vomiting, dizziness, and headaches. Additionally, these medications may increase your risk of bleeding, so it is important that you speak to your doctor before starting any course of medication in order to understand the benefits and risks involved. Your doctor will be able to provide detailed information about potential side effects so that you can make an informed decision about what’s best for you or your loved one.
Vascular and Interventional Centre is here to address your vascular needs through interventional and non-interventional customised treatments. Contact +65 6694 6270 to book an appointment with our team of well-trained vascular specialists.
You can explore our website https://www.sgvascularctr.com for more resources about conditions and our treatments. You can also visit our Facebook page (https://www.facebook.com/sgvascularctr) for additional information.

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
