What are vascular diseases?
Vascular diseases are conditions causing an abnormality in the blood vessels, mainly the arteries or veins. Any person, whether young or old, whether healthy or not, may be at risk of vascular disease. If you are unsure if you have a vascular disease, please continue reading and see a specialist to receive advice and options for vascular disease treatment Singapore.
How do I know if I have vascular disease?
Here is a brief introduction to some common vascular diseases:
● Peripheral Vascular Disease (PVD)
PVD is a condition causing the constriction (narrowing) of your blood vessels. Depending on which vessel is affected, the amount of blood flow towards the organ/limb supplied by that blood vessel becomes restricted resulting in insufficient oxygen and nutrients reaching that organ/limb to function at full capacity. The most common cause of vessel narrowing is atherosclerosis, the buildup of plaque (from fatty deposits) in the vessel walls.
While PVD can affect any part of the body such as the brain and arms, but when PVD affects the arteries supplying the lower limbs, people usually feel pain or cramps in their legs and feet. In the early stages, people with PVD may not experience any symptoms. As the disease progresses, typical symptoms of PVD may start to appear, including claudication (walking-related pain in the buttocks, hips, calves and thighs), thinning of hair on the legs, heaviness or numbness in the leg muscles, slow-healing wounds on the legs, leg cramps (when lying down and resting) and reddish or blue discolouration in the feet and toes. Do note that this list is not exclusive, and if you suspect you have PVD, early review by a doctor will help with accurate diagnosis and proper treatment, which when initiated early will help to avoid serious limb and life threatening complications later on.
● Deep Vein Thrombosis/Venous Thrombosis (DVT)
DVT occurs when a blood clot forms in one or more deep veins (veins far beneath the surface of the skin) of the body. The blood clot is usually formed in the legs or hips. This usually happens when there is pooling of blood in the veins for a significant period of time, such as during a long haul flight or during prolonged bed rest after major surgery. It can also be due to thickening of the blood in general (from infection or cancer), thus predisposing to increased risk of clots.
DVT is especially dangerous because a piece of the solid blood clot could break off and travel upwards through the bloodstream and block another important vessel – this is called an embolism. A pulmonary embolism – where the blood clot gets stuck in one of the blood vessels leading to the lung – poses the greatest risk, as it is potentially fatal. DVT can permanently damage the valves in the veins, and may cause lasting sores and swelling in the legs. However, DVT usually occurs without the affected individual showing visible symptoms.
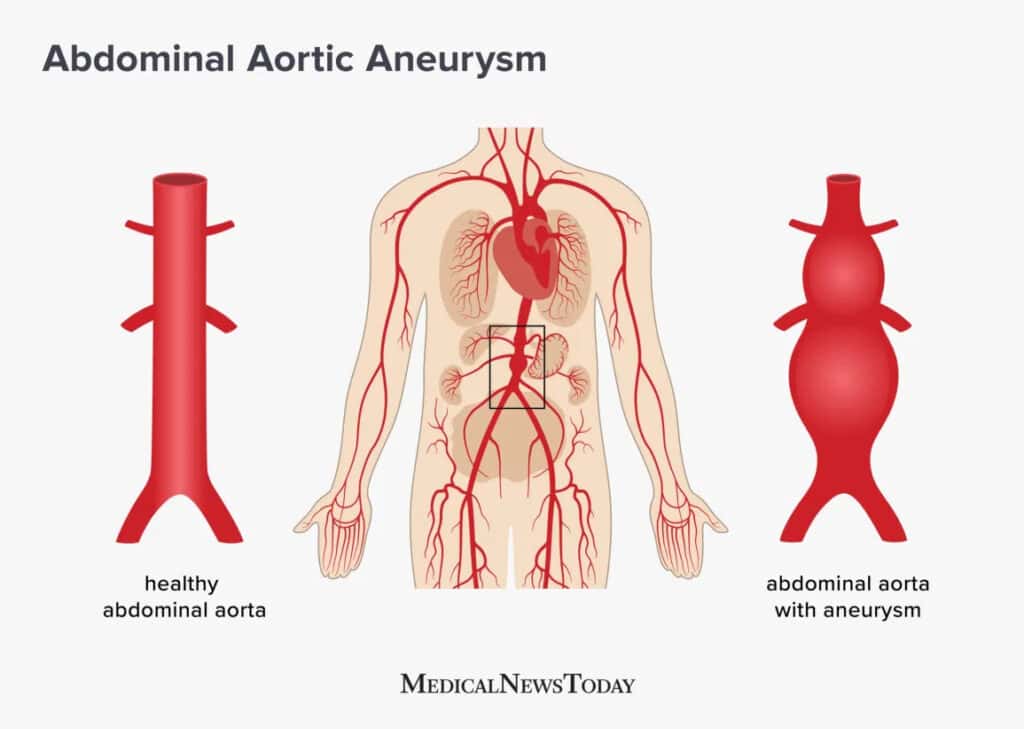
Abdominal Aortic Aneurysm (AAA)
The aorta is the main artery leading from the heart to the rest of the body. AAAs are a bulge in the aorta around the abdominal area, which pose a very serious danger of internal bleeding if they rupture. Someone may have an AAA which is getting bigger if they experience constant pain in or at the side of the belly area, back pain or feel a pulse near their belly button. An AAA is usually caused by atherosclerosis (hardening of the aorta wall), and high blood pressure (which weakens the aorta wall). The probability of getting an AAA increases with age, usage of tobacco, the presence of another aneurysm in other major blood vessels, and if one’s family member has previously had an AAA. To prevent getting AAA, one should observe a diet low in salt and saturated and trans fats, as well as stop or never start smoking. This is to reduce the chances of the onset of atherosclerosis and to maintain healthy blood pressure levels.
- Carotid Artery Disease (CAD)
CAD is similar to PVD, except that it specifically affects the carotid arteries, the main arteries leading to the brain. CAD lessens the amount of blood flowing to the brain. The cause of CAD is the same, atherosclerosis, which narrows the walls of the arteries. CAD is however much more serious than normal PVD because the brain needs a constant supply of oxygen, and if deprived for even a few minutes, brain tissue will start to die. Even worse, if narrowing of the carotid arteries is too severe or a plaque on the wall of the arteries breaks off and causes a complete blockage of blood flow, it might cause a stroke due to too little oxygenated blood reaching the brain.
There are usually no early noticeable symptoms of CAD except for occasionally a transient ischemic attack (TIA) which is temporary loss of blood flow to the brain, one of the early signs of stroke. Someone may have a TIA if they experience sudden numbness or paralysis in one of their arms, legs or side of their face and they are unable to use their limbs properly (flailing, drooping etc). If you see someone having symptoms of TIA, you should call for medical help immediately.
Treatment Options in Singapore
Treatment options for vascular diseases can be broadly categorized into medical (or non-invasive), surgical, and specialized care. Based on the type of acute or chronic vascular disease, location, severity, patient clinical condition, co-morbidities, the sizes of the centers, physician expertise, and experience in the hospital and the country, the selection of the appropriate treatment is made. Offering endovascular (minimally invasive) and open surgical treatment under one roof is often beneficial for the aorta or limbs. The availability of treatment options for vascular diseases has advanced significantly since the 1960s in the healthcare system. There have also been advances in endovascular techniques to deploy a covered stent, which has expanded the indications further and prevented life-threatening bleeding complications or occlusion of arteries, especially in complicated aortoiliac arteries in aneurysms.
• Medical Treatment: There is an excellent primary healthcare system. The government healthcare system is financially affordable for the majority of the population. Chronic limb ischemia patients present to these clinics as well. Approximately 5-12 open operations are done per one million people due to poor infrastructure availability.
• Pharmacotherapeutic Interventions: A single dose of clopidogrel 300 mg is given before and 75 mg for lifelong post-CAS patients without an additional loading dose preoperatively on anti-platelet therapy.
• Surgical Treatment: This remains the main effective tool. More or less, the nature and severity of the disease decide the choice between open and endovascular techniques.
• Specialized Care: Division between surgery and interventional treatment. Access to a vascular surgeon and an endovascular specialist within the same hospital can be a common scene in most of the large hospitals, but not in smaller private hospitals. In this scenario, depending on the diagnosis, the patient would be channeled to see either the vascular surgeon or the interventional specialist. Each of these specialists will discuss the surgical as well as the endovascular strategy and arrive at a decision, but sometimes there can be logical arguments. Of late, there has been a trend in coordinated decision-making to bring both specialists together and try to create universal standardized treatment guidelines.
Medical Interventions
The various classes of drugs and devices used in trials are also summarized in the context of the year and level of evidence available. Across a range of different outcome measures including death from any cause, large-vessel and small-vessel disease complications, pharmacological treatments can be subdivided into four main areas: antihypertensives, stroke-specific medical interventions to target hemodynamic or functional neurovascular protection effects, anticoagulants, and potent statins.
Control of high blood pressure has long been established in reducing the risk of developing cerebrovascular, aneurysmal, and peripheral arterial system complications. There is strong evidence for the use of different drug registrations of ARBs, calcium-channel blockers, and thiazides in reducing the risks of first stroke, principally hemorrhagic stroke. In general, stroke patients require more hemodynamic protection and neurovascular functionality while healthy randomized patients require neurovascular protection. The available stroke outcome data show that different antihypertensive drug classes have various degrees of hemodynamic neuroprotective value except the blocker group that is neuroprotective. With extrapolation from intervention trial data, the current best buys are the ARBs for post-stroke types and calcium-channel blockers in the costs and health benefits for high-risk pre-stroke patients.
Pharmacotherapy individualization is the key principle in drug planning of any sort even with cost-effectiveness efficacy. Emerging work on thrombolysis and interventional clot/device retrieval endovascular intervention influences the clinician’s approach to acute ischemic stroke and their potential for secondary prevention or risk of vessel dissection in hyperacute ischemic stroke. All acute and aggressive multi-drug intervention therapies except thrombolysis have to be taken with extreme caution in fractured neck of femur medical acute elderly patients. In patients with valvular replacement and atrial flutter cases, the INR ranges are clearly defined and the use of NOACs needs further study but are being used in anticoagulant aspirin takers. This would be applicable to many multiple differing drugs cocktail type medical scenarios as a consequence, although multiple drug prescription is acceptable following active intervention in high-risk patients. Given our present-day hospital cost-effective care hours, it is not possible to deploy extensive personal genomics therapy profiles and patient acceptance of such care by all may be problematic with extreme costs. The guideline recommendations have swung to including an aspirin-dipyridamole combination following secondary prevention stroke. The combination is superior for ischemic vascular protection over clopidogrel, and it is equal to clopidogrel but in excess of 10% more cost-effective for therapy alone in asymptomatic peripheral carotid revascularization. Personal lifestyle planning is a mandatory and potentially even the most useful form of treatment. This general category of high-risk patients after initial antiplatelet thrombolysis, immediate revascularization, and within two years hypertension control attracts lifestyle therapy, especially of collateral vessel boosting therapeutic aid. Following a TIA/stroke and/or peripheral arterial insufficiency events and after therapy trials have demonstrated an effect, i.e., the great bulk of acute ischemic cerebrovascular disease patients or peripheral artery occlusive disease, mini-stroke intervention therapy categories.
Surgical Procedures
Common surgical procedures used to treat vascular diseases in Singapore include: carotid endarterectomy, aortic aneurysm repair, surgical re-implantation of the superior mesenteric artery, subclavian to carotid transposition, amputations, and lower limb surgical revascularization. Each procedure is an operation to treat a particular group of conditions. Post-operatively, patients will receive close monitoring, and in certain cases, post-procedure imaging may be needed to ensure the surgery was successful. The team performs an increasing proportion of potentially risky endovascular and vascular procedures in elderly patients or younger patients with complex comorbidities in multidisciplinary settings, with input from a number of different medical specialists. The decision to operate will often involve a discussion with the patient about their comorbidities and their severity. The patient’s preferences will also be taken into account. The follow-up imaging results of re-implantation of the subclavian to carotid transposition are being assessed with vascular surgeons. This topic will be shared to further engage the cardiac and vascular interventionists on their treatment preferences and results between the two characteristics.
In most circumstances, patients will undergo surgery after discussing suitable treatment options and having a clear understanding of procedures and their risks. An exception is if there is a high risk of dying from an operation. In this case, surgery may not be offered or the number of replacement grafts available will be severely limited. Patients may also be offered other surgical treatments or alternative non-surgical options. Several important outcomes are measured to help compare surgical, endovascular, and conservative management of arterial aneurysmal disease. In summary, many of the major large vessel and aneurysm treatments are now performed in the public healthcare sector. One-stop care is frequently provided through combined clinic services, and packing and stent interventions have become the primary treatment modalities for a number of diseases. The outcomes are encouraging and suitably monitored. Pre-procedural embolization is infrequent and often administered in the context of lower extremity amputations. The choice of treatment in the clinics varies by disease and patient preference; the best results are typically seen with aneurysmal surgery at most clinics. Follow-up after hospital discharge is often undertaken at specific medical or surgical clinics. Some of these clinics provide one-stop care including imaging and surgical consultations where necessary. Overall, various aspects of treatment including outcomes, wound healing, quality of life, and general clinical progress are carefully analyzed to support and promote standard operating procedures of vascular disease treatment throughout the healthcare delivery system.
Preventive Measures
Pre-disease stage: It is critical to identify individuals at high risk of developing vascular diseases before onset, so that early preventive management can be deployed. In Singapore, preventive public health initiatives have resulted in the reduction of disease prevalence. Thus, health interventions, the early detection of risk factors, and early treatment (prevention of the progression of the risk factors), when net health benefits are high, are generally recommended. A preventive ‘pre-disease’ approach is more cost-effective than disease intervention, as it involves considerably lesser costs.
Many preventive health services are expensive in terms of money, time, and inconvenience to the consumer, have potentially negative side effects, and have little effect on ultimate health outcomes. Strategies for high-risk prevention have been found to be less effective than strategies that combine mild population programs with high-risk approaches. That is why many preventive programs now include behavior change elements.
Evidence-based strategies: There are evidence-based preventive strategies for vascular diseases, but there is a need for a strategic shift to a proactive integrated care model using new techno-economic stochastic models and shared care for prevention. High vascular risk needs to be ascertained by a simple risk assessment of diabetics, hypertensives, and heart/cholesterol patients younger than 60. There needs to be early statin use and diet modification for high-risk clusters, intensive therapy for moderate clusters, lifestyle modification advice for others at risk, and government policies that force food corporations and eateries to have less salt and fewer high-energy food choices. Ultimate prevention of vascular disease will come from community – rather than individual – intervention. This will require cultural change, social capital, personal and institutional development, and a transdisciplinary approach.
Lifestyle Modifications
Every individual should adopt a healthy lifestyle that can prevent and decrease their risk of vascular diseases. Physical activity increases blood circulation to the heart and decreases the overall risk of vascular diseases. Regular physical activity is recommended for at least 150-300 minutes of moderate-intensity aerobic activity a week. Stress-reducing activities, sleep hygiene, and self-care, like reducing caffeine intake and limiting exposure to electronic devices before bedtime, can prevent vascular diseases. To date, smoking cessation remains the single most important preventive strategy for decreasing the risk of developing hypertension, dyslipidemia, type 2 diabetes mellitus, and hence vascular diseases. Excess weight, in particular, abdominal obesity, will lead to an increased risk of developing vascular diseases. Lifestyle modifications should encourage healthy eating practices and teach how to make healthier choices to maintain a healthy weight.
Annual health screening for all working adults and seniors is recommended. This is to allow early detection of any risk factors for disease development and to allow proactive management measures to be executed. Advice or guidance can be obtained through health promotion initiatives designed to encourage individuals to be more physically active, healthy, and reduce health risks. Benefits of being physically active are accumulated throughout the day; as such, practitioners can promote the total accumulated time spent by patients in physical activity and exercises. They can set small goals for increasing physical activity each day and slowly increase active time spent in exercises. Incorporate the management plan for lifestyle changes at each follow-up visit and the possible use of mobile health applications or devices for self-monitored health assessment. The creation of a supportive environment is necessary for the adoption and maintenance of a healthy lifestyle. For instance, the workplace leader, as a key influencer, can promote workplace health by creating a healthy environment to encourage physical activity and active commuting. There is also an increasing trend for gym facilities to be provided at workplace premises.
Dietary Recommendations
Dietary strategies can effectively help manage blood pressure and cholesterol levels, as well as overall cardiovascular health. A diet rich in fruits, vegetables, whole grains, and heart-healthy fats can help protect your arteries. Below are dietary recommendations that can lead to improvements in vascular health:
– Fruits and vegetables that are colorful and have low natural sugar content are advised.
– Whole grains such as oats are beneficial in maintaining healthy cholesterol levels.
– Legumes (beans, lentils, and chickpeas) are a rich source of dietary fiber and plant-based protein that can help to reduce blood cholesterol levels.
– Healthy fats such as avocado and those found in fatty fish, olive oil, and nuts can help to reduce the risk of high cholesterol, blood pressure, and heart diseases.
– People are also advised to hydrate with water and reduce the consumption of beverages with added sugars and alcohol.
– The intake of processed foods such as small goods and fried items, as well as canned foods and healthier alternatives, will help to reduce the amount of noise in your diet along with your salt and sugar intake.
A local dietary guide compiled according to the three main ethnicities in Singapore advocates a mainly plant-based diet filled with various fruits and vegetables, whole grains, low-fat dairy products, and modest amounts of meat. It is important to understand that small dietary changes can lead to vast improvements in your vascular health, and if in doubt, always speak to a professional. Diets that include multiple lifestyle modifications, such as increased physical activity aimed for at least 150 minutes per week, including resistance training on two days, quitting smoking, watching alcohol intake, and reducing sodium or sugar to protect heart health, can help people lower their blood pressure, cholesterol, and glucose.
Overall, nutritional strategies provide additional benefits outside of pharmacological medication due to a reduction not only in interdependence of major health benefits such as cholesterol lowering, improved blood glucose control, and functional capacity. Any dietician or pharmacological plan to reduce global vascular risk may require additional adjustments in food intake to avoid nutrient-drug interaction. Many of the protective benefits of nutrients in foods and functional dietary approaches are amenable to individuals from various demographics and can be adapted to include local and cultural specialties for those residing here. Specialized services and support are required in selecting complementary dietary approaches that align with integrative lifestyle modifications. Nutritional education, in some cases, involves strategies in cooperation with diets from professional health behaviors, self-efficacy, and transition to ongoing care. As with all dietary modifications, a balanced approach to mental and social health is also conducted.
Do I need to go for vascular disease treatment Singapore?
For most vascular diseases, it is recommended that you see a vascular specialist in order to have a comprehensive assessment and make an accurate diagnosis to guide appropriate treatment.
If left untreated, vascular diseases may escalate quickly and prove fatal. Feel free to book an appointment or contact us if you have any concerns!
