Overview of Carotid Artery Disease: Causes, Symptoms, and Risk Factors
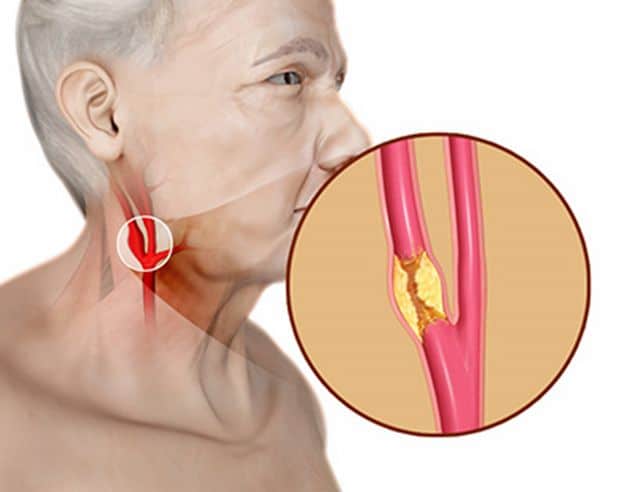
The carotid arteries are located on either side of your neck and supply oxygenated blood to your brain from your heart. These vessels can become narrowed or blocked due to plaque deposits caused by atherosclerosis (fatty deposits in the walls of the arteries). When this happens, it is referred to as carotid artery disease (CAD). CAD can reduce the blood supply to the brain, thus leading to stroke or permanent brain damage.
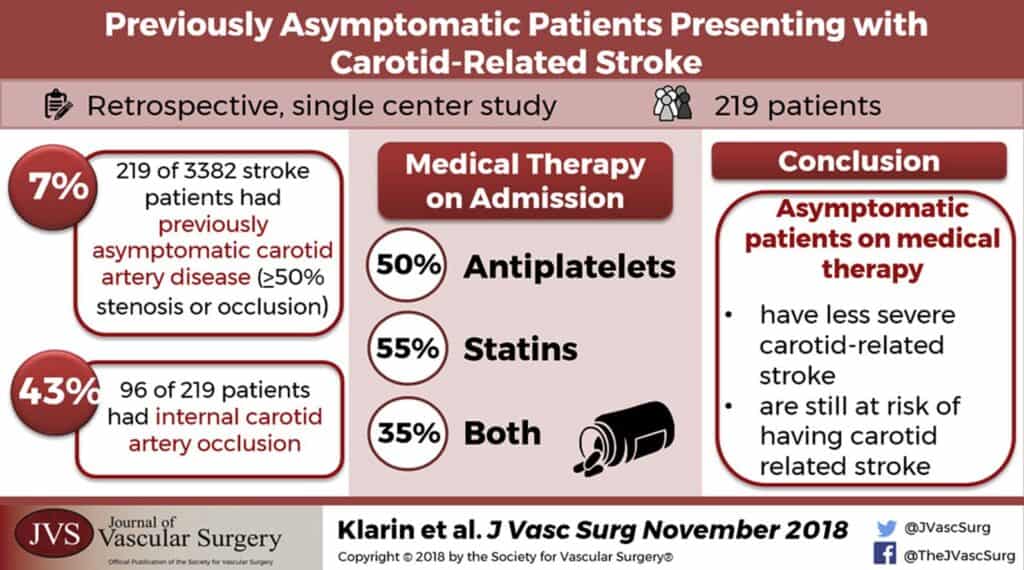
The most common risk factors for CAD include high cholesterol levels, uncontrolled diabetes, hypertension (high blood pressure), smoking, and obesity. It’s important for anyone at risk of developing the condition to be aware that many patients do not experience any symptoms until an irreversible stroke occurs. Thus it is important for patients (especially those with risk factors) to have regular health screening specifically for CAD to detect it early and initiate treatment before a debilitating stroke happens.
(https://www.sydneyvascularsurgery.com.au/carotid-artery-disease.html)
Diagnosing Carotid Artery Disease: Tests and Imaging Scans
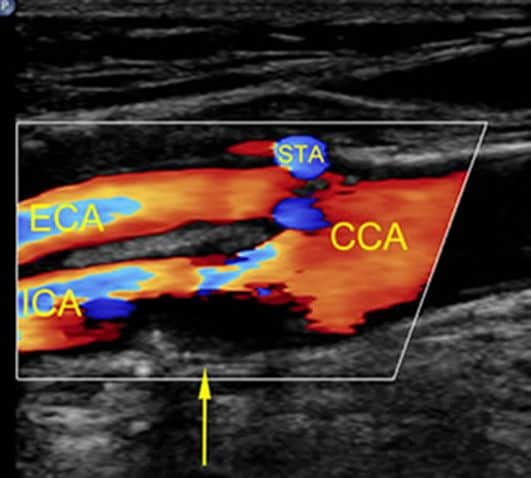
Most of the time CAD is asymptomatic (no signs or symptoms) until it is too late, when a stroke occurs. Thus screening for CAD prior to any symptoms onset in people, especially those with risk factors is the best option so that treatment can be initiated early to reduce the risk of a stroke. The primary test used by doctors when diagnosing an individual with CAD is a Doppler ultrasound scan, which uses sound waves to create images that show if there are blockages in the internal carotids and their degree of severity if present. Other tests that help diagnose CAD include magnetic resonance angiography (MRA), and carotid angiography. Usually more than one imaging modality is required to obtain all necessary information required to make accurate treatment decisions.
(https://bestpractice.bmj.com/topics/en-us/1205)
Lifestyle Changes to Reduce Your Risk of Carotid Artery Disease
It’s important for those who are at risk of developing CAD (due to age, high cholesterol levels, diabetes, etc.) to take steps to reduce their risk as much as possible by making lifestyle changes such as:
- eating a balanced diet that is low in saturated fat and sugar.
- exercising regularly
- maintaining good blood pressure through low salt diet and regular exercise
- quitting smoking if you are a smoker.
Lifestyle changes can lower the risk of developing CAD, and also lower the chance of CAD worsening leading to a stroke. However please note that lifestyle changes alone are insufficient once CAD has developed, and a comprehensive evaluation and appropriate medical treatment is still required to adequately reduce the risk of a debilitating stroke.
Treatments for Carotid Artery Disease
In most cases, medications will also be needed alongside lifestyle changes when treating established carotid artery disease. They can help reduce the amount of cholesterol and lipids (fatty substances) circulating through the bloodstream, which reduces plaque deposits in your internal carotid arteries.
- Statins are a group of medications that inhibit an enzyme required to produce cholesterol, and they’ve been found to reduce cholesterol levels significantly when taken regularly.
- Other prescription drugs used in CAD include ACE inhibitors, beta blockers, calcium channel blockers, and antiplatelets; these prevent new clot formations from forming along any narrowed areas of the artery walls.
If there are concerning signs associated with the CAD (such as microemboli seen coming from the plaque, or critical stenosis >70%), medications and lifestyle changes will be inadequate at preventing a serious stroke. Surgery is usually recommended in such instances.
(https://www.mayoclinic.org/tests-procedures/carotid-angioplasty-and-stenting/about/pac-20385111)
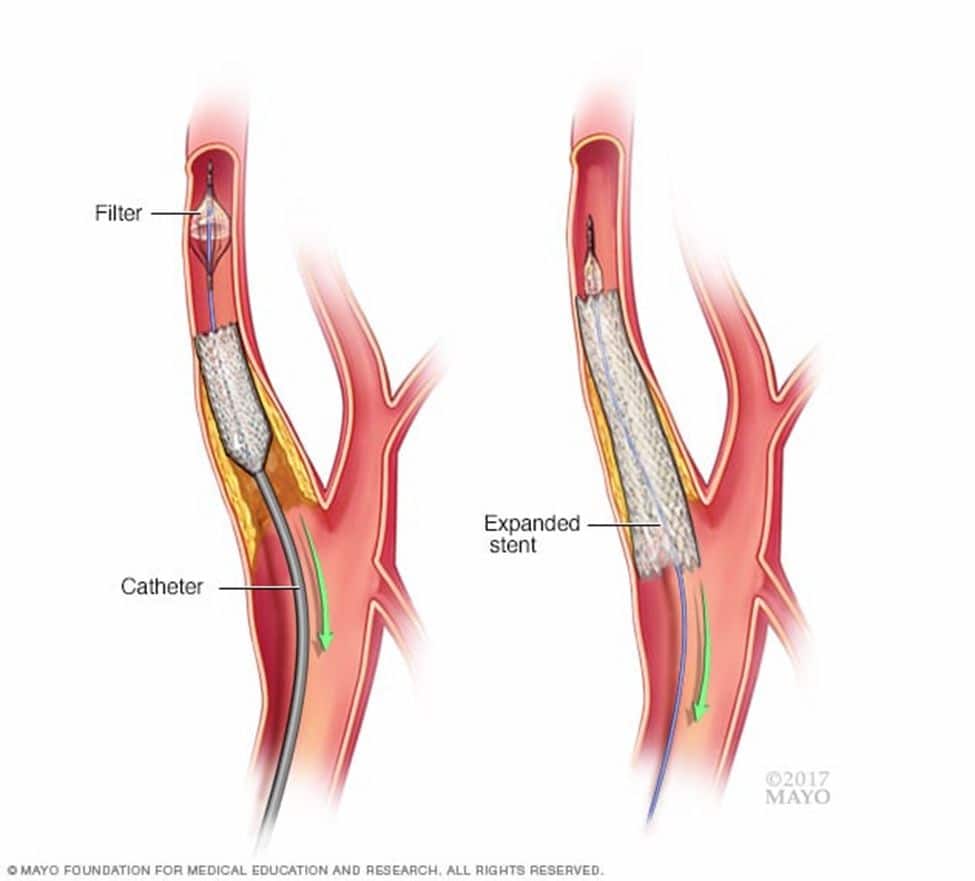
Surgery can be either open (carotid endarterectomy surgery) or endovascular (involving ballooning and stenting). Endovascular Carotid artery stenting is a relatively new procedure, involving introducing a flexible wire mesh (aka stent) via a small puncture in the groin and positioning the stent across the diseased carotid artery. This serves to compress the atherosclerotic plaque to the side, thus opening up the narrowed blood vessel and improving blood flow to the brain, thus reducing the risk of a stroke.
(https://www.healthlinkbc.ca/health-topics/carotid-endarterectomy)
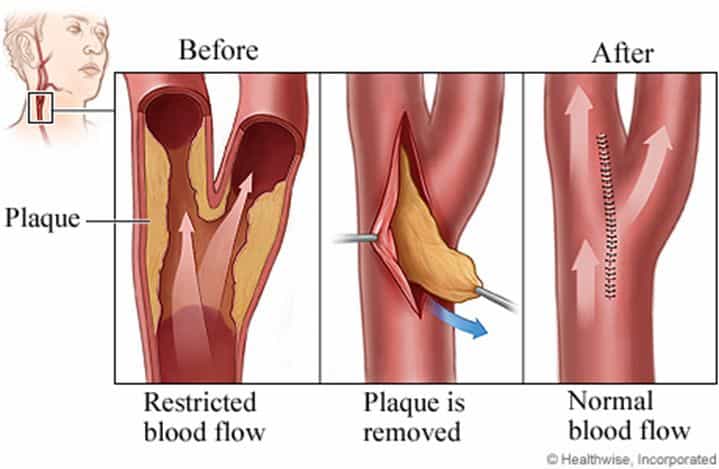
Open surgery (Endarterectomy) is the traditional surgical option for treating carotid artery disease. This procedure involves an incision along the neck and accessing the carotid artery before removing the blockage inside the artery and restoring proper blood flow. There are pros and cons to each surgical approach and an experienced Vascular surgeon experienced in both modalities will be able to advise which option is more suitable for your situation.
Expectations and Preparations for Carotid Artery Disease Treatment
The preparation and recovery after CAD treatment largely depends on which surgery (open vs endovascular) was performed. Good blood pressure control and adequate anticoagulation is generally required to ensure good outcomes.
Recovery after endovascular surgery is generally quicker as it is minimally invasive, and most patients can discharge after 1-2 days of hospital stay post-operatively. A small tube (drain) may be placed in the neck wound after open endarterectomy surgery, and this is usually removed after 1-2 days. The neck incision wound will heal in 2 weeks if there are no complications.
It is imperative to take all prescribed medications after any surgery to reduce risk of infection and stroke complications.
(https://www.sciencedirect.com/science/article/pii/S0741521418308279)
How to Find the Right Doctor for Carotid Artery Disease Treatment
CAD surgery is considered high risk, with the main concern being a stroke during the surgery and in the immediate recovery phase. An experienced Vascular surgeon will conduct a systematic evaluation of all the blood vessels going to the brain (internal carotid and vertebral arteries), the blood vessels within the brain itself (Circle of Willis etc), as well as the morphology of the CAD atherosclerotic plaque to advise on the best treatment for your particular situation, be it medications and with/without surgery (open vs endovascular).
An acceptable peri-operative stroke rate after CAD surgery is in the region of <3% with very good centers having a stroke rate of 1% or less. By asking for the perioperative stroke rate, one can determine how competent the surgeon is at CAD treatment.
The Role of Nutrition and Exercise in Carotid Artery Disease Treatment
- Nutrition plays an important role in carotid artery disease treatment. Eating a diet rich in fruits, vegetables, and whole grains and low in saturated and trans fats can help reduce cholesterol levels and reduce the risk of carotid artery disease. Additionally, getting regular physical activity can help reduce cholesterol levels and reduce the risk of stroke.
- Exercise is an important part of carotid artery disease treatment. It can help reduce blood pressure and cholesterol levels, as well as help maintain a healthy weight. Additionally, exercise can help reduce stress and improve mental health. It’s important to talk to your doctor about an exercise plan that is right for you.
(https://www.phillyvoice.com/difference-regular-strokes-ministrokes-059991/)
Life After Carotid Artery Disease Treatment
Once you’ve completed carotid artery disease treatment, it’s important to lead a normal life. This includes following your doctor’s instructions for care and getting regular check-ups and taking all necessary medications. Additionally, it’s important to maintain a healthy lifestyle and to make any necessary lifestyle changes, such as quitting smoking, eating a healthy diet, and getting regular physical activity.
FAQs
Carotid artery disease is a condition that develops when the carotid arteries, which are the major blood vessels in the neck, become narrowed or blocked due to the buildup of plaque. Common symptoms include dizziness, headaches, visual disturbance, arms/leg weakness and stroke.
The risk factors for carotid artery disease include age, family history, high blood pressure, high cholesterol, diabetes, smoking, and obesity.
Treatments for carotid artery disease include medications, lifestyle changes, and surgery (either open or endovascular).
Yes, making lifestyle changes can help reduce the risk of carotid artery disease. These lifestyle changes include eating a healthy diet, getting regular physical activity, quitting smoking, and maintaining a healthy weight.
Yes, eating a diet rich in fruits, vegetables, and whole grains and low in saturated and trans fats can help reduce cholesterol levels and reduce the risk of carotid artery disease.
Tests used to identify carotid artery disease include physical exams and imaging tests, such as an ultrasound, CT scan, or MRI.
It’s important to seek treatment promptly after diagnosis, as carotid artery disease can lead to serious complications if left untreated.
It depends on your insurance plan, but the treatment is considered a medical necessity and should be covered by most good insurance plans.
Patients with carotid artery disease should be monitored regularly, as this condition can lead to serious complications if left untreated.
The long-term effects of carotid artery disease can include stroke through decreased blood flow to the brain, ruptured plaques, paralysis, loss of speech, and death.
Vascular and Interventional Centre is here to address your vascular needs through interventional and non-interventional customised treatments. Contact +65 6694 6270 to book an appointment with our team of well-trained vascular specialists.
You can explore our website https://www.sgvascularctr.com for more resources about conditions and our treatments. You can also visit our Facebook page (https://www.facebook.com/sgvascularctr) for additional information.
References
[1] https://www.sgvascularctr.com/service/carotid-artery-disease/
[2] https://www.sgvascularctr.com/how-to-prevent-diseases-related-to-your-veins/
[3] https://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/in-depth/statins/art-20045772/
[4] https://pubmed.ncbi.nlm.nih.gov/11281235/
[5] https://pubmed.ncbi.nlm.nih.gov/31705988/

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
