
VASCULAR ACCESS FOR HAEMODIALYSIS
Vascular access refers to the method in which a tube is inserted into a patient’s bloodstream to grant easy access to their veins. This method enables kidney failure patients to undergo haemodialysis. No matter the cause of kidney failure, every dialysis patient must undergo vascular access. The access allows blood to travel through these tubes into the dialysis machine where it can be cleaned and returned into the bloodstream.
There are three types of vascular access:
- Central venous catheter
- Arteriovenous Fistula (AVF)
- Arteriovenous Graft (AVG)
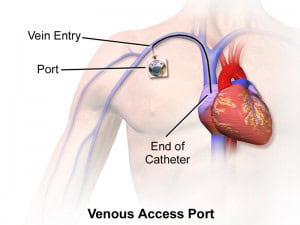
CENTRAL VENOUS CATHETER/PERMANENT CATHETER
Catheter access sometimes called a Permanent Catheter or CVC (central venous catheter), is access where a Y-shaped catheter is placed into a central vein (usually the jugular or femoral vein) to allow blood to be withdrawn from one lumen to enter the dialysis circuit, then be returned via the other lumen. These catheters can be inserted in an outpatient clinic in a minimally invasive way.
There are two types of CVCs, tunnelled and non-tunnelled:
- Non-tunnelled catheter access is for short-term access (up to about 14 days), and the catheter emerges from the skin at the site of entry into the vein.
- Tunnelled catheter (also known as Permanent Catheters) access is usually more long term, involves a longer catheter, which is tunnelled under the skin from the point of insertion in the vein to an exit site some distance away. It is usually placed in the internal jugular vein in the neck, and the exit site is generally on the chest wall. The tunnel acts as a barrier to invading bacteria. Although called a Perm Cath, such tunnelled catheters are designed for short- to medium-term access because the infection is still a frequent problem. We do not recommend placing a Perm Cath for more than six months.
CENTRAL VEIN STENOSIS (CVS) AS A RESULT OF PERMCATH COMPLICATION/INFECTION
CVS is a serious, and not uncommon, a problem associated with the long-term use of Perm Caths. As the catheter is a foreign body in the vein, it often provokes an inflammatory reaction in the vein wall. This results in the vein becoming scarred and narrowing, which causes a blockage to the blood flow. CVS has been known to cause symptoms such as swelling in the face, neck, chest and/or the upper limbs.
OUR TREATMENTS
Treatment of CVS requires a procedure known as a Venoplasty, a treatment used to open clogged veins. In this procedure, a balloon is inserted into the vein through a wire and inflated in order to open up the vein. Sometimes, if the narrowing is resistant to the balloon dilatation, then a stent (metal supporting strut) may be placed across it to keep the vein open. The Venoplasty and Stenting can be done under local anaesthesia or mild sedation and as a day surgery procedure.
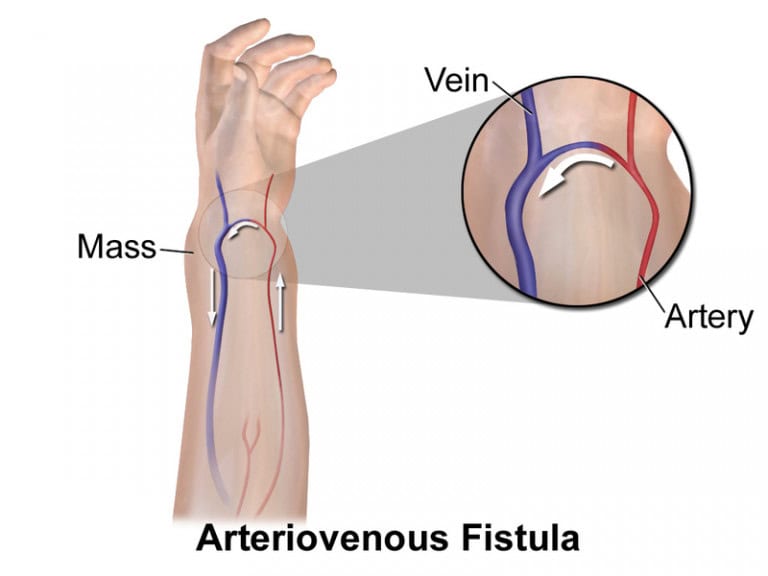
ARTERIOVENOUS FISTULA (AVF)
An AVF is the surgical connection of an artery and a vein. It is the preferred access method and can last for a longer time than a stent or catheter. It is created by stitching an artery and a vein together, usually in the non-dominant arm in either the hand, forearm or elbow.
AVFs have lower infection rates as no foreign materials are left in the body for extended periods of time. While it may take up to 8-12 weeks to mature and become fully functional, it is considered to be more effective than other methods as it allows for a higher rate of blood flow and more effective dialysis. On the whole, an AVF has fewer complications than additional accesses. An AVF is usually done under local anaesthesia and as a day surgery.
ARTERIOVENOUS GRAFT (AVG)
Similar to an AVF, an AVG procedure connects an artery with a vein. However, it uses an artificial vessel made of synthetic materials to join them instead. An AVG is inserted when a patient’s veins are too small or blocked. While an AVG can mature faster than fistulas, developing as early as 48 hours, it is more prone to an infection and will generally be changed once every few years.
