Understanding The Impact of Varicose Veins on Singaporeans
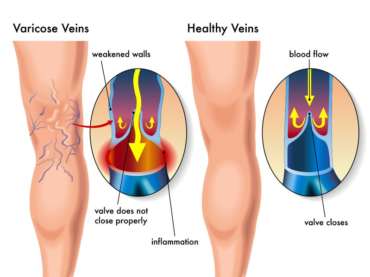
Varicose veins, and their milder form known as spider veins, are swollen and enlarged blood vessels that commonly appear in the legs due to increased pressure when standing and walking upright. These visible veins result from weakened valves that malfunction, allowing blood to flow backward and pool in the veins. This congestion leads to twisting and lengthening of the affected veins, often causing discomfort and pain.
Varicose veins can lead to a variety of unpleasant symptoms. The most common of these is a dull ache, often accompanied by a sensation of heaviness or throbbing in the legs. These symptoms can be pronounced after long periods of standing or sitting. Additionally, individuals with varicose veins may experience muscle cramps, particularly at night, and a heightened sense of leg fatigue. In some cases, the condition can lead to itchiness and skin changes in the affected areas.

(image source: https://www.healthline.com/health/varicose-veins)
While the exact cause of varicose veins isn’t always clear, several risk factors can increase the likelihood of developing them. Genetics play a significant role; if your parents or grandparents had varicose veins, you are more likely to develop them as well. Other contributing factors include age, as veins naturally lose elasticity and valve function over time. Gender is another factor, with women being more prone to varicose veins, especially during pregnancy and hormonal changes. Prolonged periods of standing or sitting, obesity, and lack of physical activity can also elevate your risk.
Fortunately, several treatment options are available for varicose veins, ranging from minimally invasive measures to more traditional procedures. Compression stockings are a commonly recommended non-invasive approach that helps alleviate symptoms by promoting better blood flow. Lifestyle modifications, such as regular exercise and maintaining a healthy weight, can also assist in managing the condition. For more severe cases or when conservative treatments prove ineffective, medical interventions like sclerotherapy (injecting a solution into the veins to close them off) may be necessary. In extreme cases, surgical procedures, such as high-tie ligation and vein stripping, can be considered.
Exploring the Symptoms of Varicose Veins
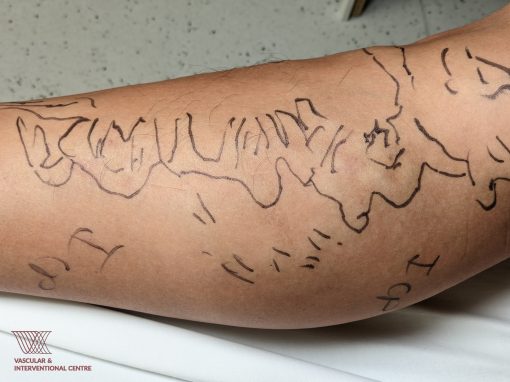
One of the most common symptom of varicose veins is the appearance of several networks of red, purple, or blue vessels, which are visible beneath the skin. You may experience a sensation of heaviness or swelling in their legs, which can worsen after extended periods of standing or sitting. Patients often experience persistent leg ache. Varicose veins may cause your skin color to change. Some patches of your skin may turn darker, especially around the affected veins. Another common symptom is itchy skin surrounding the veins, which can be a source of discomfort and irritation.
(image source: https://mcquaidvein.com/vein-problems/varicose-veins/)
Common Causes & Risk Factors of Varicose Veins
- The likelihood of developing varicose veins tends to rise with age, as the wear and tear on vein valves can lead to blood reflux and pooling.
- Varicose veins are more prevalent in females, often associated with hormonal changes during pregnancy, menstruation, or menopause that relax vein walls.
- The increased blood volume in a mother’s body during pregnancy can cause veins to enlarge to accommodate the growing fetus.
- Individuals with a family history of similar conditions have a greater predisposition to varicose veins.
- Excess weight exerts additional pressure on the veins, contributing to their development.
- Extended periods of standing, particularly in work settings, can lead to compromised blood circulation.
A Step-by-Step Process on How Vascular Surgeons Diagnose Varicose Vens
First, your healthcare provider carefully examines your legs, looking for signs of varicose veins like swelling, twisted veins, changes in skin color, or any discomfort you might be feeling. To be sure about the diagnosis, they often use an ultrasound scan. This scan helps identify which veins are working properly and which are not. Using these methods, your vascular surgeon can now figure out what’s going on with your veins and why you’re experiencing the symptoms you have. This way, you can manage any discomfort, pain, or other effects of varicose veins effectively.
(image source: https://www.sgvascularctr.com/service/vein-diseases-varicose-veins/)
Examining the Different Treatment Options for Varicose Veins
1.Conservative Non-Surgical Treatments
Conservative non-surgical treatments for varicose veins involve the use of tight compression stockings. These stockings promote better blood flow within the leg veins, offering relief from discomfort. By gently squeezing the legs, these stockings reduce the pooling of blood in the veins. While they can be effective in milder cases, individuals with more severe varicose veins and pronounced symptoms may need additional treatment and care to address their condition effectively.
2.Traditional Open Surgery
Conventional open surgery, known as high-tie ligation and vein stripping, necessitates general anesthesia and typically involves an overnight hospital stay. This method is often linked to more significant discomfort and a slower recovery process.
3.Minimally Invasive Procedures
Minimally invasive procedures offer several advantages over traditional surgery. Patients can expect quicker recovery times and less pain compared to open surgery. As opposed to open surgery, minimally invasive procedures are performed through tiny incisions. This technology allows for the insertion of probes through small punctures to seal off the vein. These procedures are typically done as day surgery, allowing patients to return to their daily activities without the need for a lengthy hospital stay. Local anesthesia or light sedation is used, and various methods, including heat, mechanical, or chemical techniques, are employed to seal the vein.
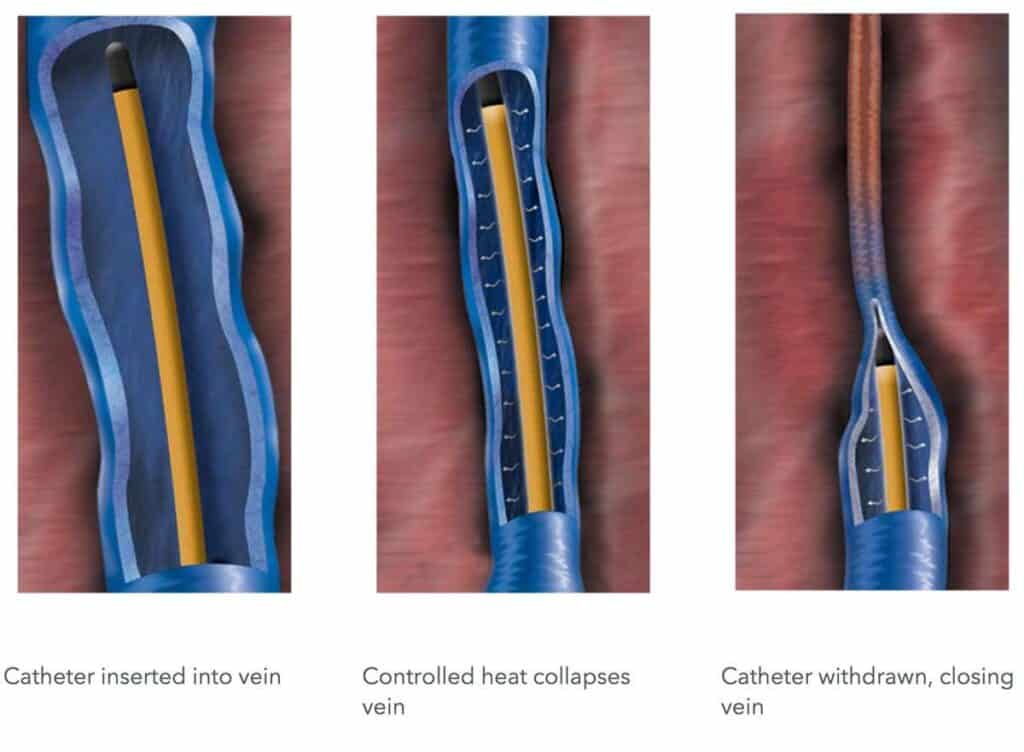
(image source: https://theswiftinstitute.com/radiofrequency-ablation-closurefast/)
The Vascular & Interventional Centre in Singapore offers treatment methods such as:
- Radio Frequency Ablation (RFA): This outpatient procedure uses radiofrequency energy to heat and damage the vein wall. It is a fast and safe minimally invasive procedure.
- Venseal™/VenaBlock Glue Closure: A small amount of specialized medical adhesive permanently seals varicose veins. This reroutes blood to nearby healthy veins, providing relief. The procedure is comfortable and typically takes 15-20 minutes.
- Clarivein™ Mechanochemical Ablation: This technique combines mechanical destruction of veins with the injection of sclerosant to seal the vein. A rotating wire damages the vein’s innermost layer while sclerosant seals it off. It’s a painless method with fewer local anesthetic injections and no risk of heat-related nerve damage.
- Cryo-Laser and Cryo-Sclerotherapy (CLaCs): Suitable for spider veins, this procedure combines transdermal laser and injection sclerotherapy using a chemical sclerosant while cooling the skin. It minimizes scarring and pigmentation after surgery, targeting affected blood vessels beneath the skin using advanced technology for safe and effective results.
To find out if the procedure is right for you, you may request a consultation with one of our doctors to help you understand your options and choose the optimal treatment.
The Benefits and Risks of Varicose Vein Treatment
1.Benefits of Varicose Vein Treatment:
- Varicose vein treatment can alleviate discomfort, aching, and heaviness in the legs, improving overall quality of life.
- The procedure can enhance the appearance of the legs by reducing the visibility of varicose veins and associated skin discoloration.
- Treatment can prevent potential complications like blood clots or skin ulcers that may arise from untreated varicose veins.
2.Risks of Varicose Vein Treatment:
- There is a slight risk of infection at the treatment site, but it is relatively low.
- Some patients may experience bruising or swelling in the treated area, which usually subsides over time.
- In rare cases, individuals may have allergic reactions to medications or materials used in the treatment.
Finding a Varicose Vein Treatment Provider in Singapore
The Vascular & Interventional Centre in Singapore houses a team of skilled vascular surgeons and a dedicated medical staff who are well-equipped to provide effective treatment for varicose veins. Our team specializes in minimally invasive procedures. These procedures not only alleviate the discomfort and pain associated with varicose veins but also result in quicker recovery times compared to traditional surgical approaches. With a commitment to patient well-being and comfort, VIC ensures that individuals seeking treatment for varicose veins receive quality care and suitable solutions tailored to their specific needs.
Questions to Ask Your Vascular Surgeon About Varicose Veins
1.What is the cause of my varicose veins and is treatment necessary for my condition?
2.What are the symptoms, and how can I differentiate them from other conditions?
3.What lifestyle changes can help manage varicose veins?
4.What are the treatment options, and which is best for me?
5.What are the risks and benefits of each treatment?
6.How do you determine the most suitable treatment for my condition?
7.What’s the expected outcome, and how soon will I see results?
8.Are there potential complications from this treatment?
9.What’s the recovery time, and when can I resume normal activities?
10.Are there any long-term considerations after treatment?
If you have varicose veins or are at risk of developing them, it’s best to reach out to a vascular surgeon. Early detection and management can alleviate discomfort, prevent complications, and improve your overall well-being. Don’t hesitate to consult with a vascular surgeon to discuss your varicose vein concerns and explore suitable treatment options for you.
FAQ:
Varicose veins are primarily caused by weakened or damaged vein valves, which lead to the pooling of blood and the formation of swollen veins.
Symptoms of varicose veins can include visible twisted and swollen veins, aching or discomfort in the legs, skin discoloration, and itching around the affected area.
There are several treatment options for varicose veins, including minimally invasive procedures like radiofrequency ablation and sclerotherapy, as well as traditional surgery such as vein stripping.
The coverage of varicose vein treatment by insurance can vary, and it’s advisable to check with your insurance provider to determine if your specific treatment is covered.
During varicose vein treatment, you can expect a relatively short and minimally invasive procedure, with post-treatment recovery often involving minimal discomfort and a quick return to normal activities.
Sclerotherapy is a medical procedure used to treat varicose veins and spider veins. It involves injecting a solution directly into the affected veins, which causes them to collapse and eventually fade from view.
The injected solution irritates the lining of the blood vessels, leading to inflammation and closure of the vein. Over time, the body absorbs the treated vein, effectively eliminating it from circulation.
Sclerotherapy is primarily used for treating varicose veins and spider veins, which are smaller and less severe than varicose veins.
Minimally invasive: The procedure requires no incisions and can often be performed in a doctor’s office.
Quick recovery: Patients can typically resume normal activities shortly after treatment.
Effective results: Many patients see significant improvement in the appearance of their veins after just one session.
A typical session lasts about 30 to 45 minutes, depending on the number of veins being treated.
Many patients require multiple sessions to achieve desired results, typically spaced several weeks apart.
Post-treatment, patients may experience mild discomfort or bruising but can usually return to normal activities immediately. Compression stockings may be recommended to aid recovery.
Consulting with a vascular surgeon is essential to determine if you are a suitable candidate for sclerotherapy based on your specific condition and medical history.
References:
- https://www.healthline.com/health/varicose-veins
- https://www.sgvascularctr.com/service/vein-diseases-varicose-veins/
- https://www.sgvascularctr.com/wp-content/uploads/2022/01/spider-and-varicose-veins-1.pdf

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
- Tags:
- Clacs Singapore
- laser treatment of varicose veins Singapore
- painful veins in legs Singapore
- sclerotherapy Singapore
- Spider vein treatment
- Spider vein treatment Singapore
- spider veins removal signapore
- Spider Veins Treatment Singapore
- Treatment of varicose veins
- Treatment of varicose veins Singapore
- varicose vein specialist Singapore
- Varicose veins
- Varicose Veins Doctor Singapore
- Varicose veins in legs Singapore
- Varicose veins pregnancy Singapore
- varicose veins procedure singapore
- Varicose Veins Singapore
- Varicose veins surgery
- Varicose veins surgery Singapore
- varicose veins treatment
- varicose veins treatment singapore
