What is an aortic aneurysm?
The aorta is a crucial component of the human circulatory system, serving as a major blood vessel that plays a fundamental role in delivering oxygen-rich blood to various parts of the body. The aorta can be thought of as the main highway of the circulatory system, carrying freshly oxygenated blood away from the heart and distributing it to the different regions and cells that require oxygen and nutrients to function properly.
(https://medlineplus.gov/ency/article/000162.htm)
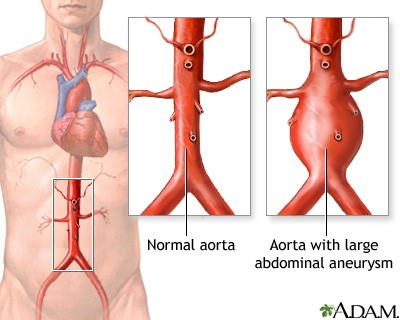
An aortic aneurysm happens when a section on the aorta’s wall protrudes and bulges outwards, similar to a balloon. This condition can manifest either in the chest (thoracic aneurysm), at various points along the aorta, such as in the abdomen (abdominal aortic aneurysm), and between the chest and abdomen (thoracoabdominal aortic aneurysm). These complications may include not only aortic aneurysms but also aortic dissections. An aortic dissection is a condition where a tear develops in the aorta’s wall, allowing blood to flow between its muscle layers and splitting it into two channels instead of one. This disruption can impair blood flow to vital branches and organs supplied by the aorta, such as the intestines, kidneys, and legs, potentially leading to organ failure and severe health complications.
Common Causes and Risk Factors of Aortic Aneurysm
Conditions involving the aorta, including aortic aneurysms and dissections, can be triggered by various factors. High blood pressure, which exerts increased force on artery walls, can weaken them over time. Genetic conditions, such as Marfan’s Syndrome, can compromise the body’s ability to produce healthy connective tissue, making the aorta more susceptible to stretching. Additionally, high cholesterol and atherosclerosis can lead to plaque buildup, causing inflammation in and around the aorta and other blood vessels. Inflammatory conditions like vasculitis can also contribute. Traumatic events, such as car accidents, are a potential risk. Smoking plays a significant role, with chronic smokers constituting a substantial portion of abdominal aortic aneurysm cases. Those at higher risk often include older males with a history of long-term hypertension or heart disease, individuals with congenital soft tissue disorders, and those with a family history of aortic aneurysms and dissections. These factors collectively underscore the importance of proactive health management and lifestyle choices in preventing aortic complications.
(https://gesund.bund.de/en/abdominal-aortic-aneurysm)
Symptoms of an Aortic Aneurysm & When to Seek Medical Attention
Aortic aneurysms are sometimes known as “silent killers” as they usually do not cause any signs or symptoms until a sudden life-threatening rupture occurs. Thus it is imperative that anyone with known risk factors should visit a Vascular surgeon to be screened for the presence of an aortic aneurysm even before there are any signs or symptoms.
If you find yourself experiencing symptoms including persistent and severe pain in areas like the chest or abdomen it should raise immediate concern and it is imperative that you promptly seek emergency medical attention, as these could be signs of an impending aortic aneurysm rupture.
Diagnosis and Tests for Aortic Aneurysm
Diagnosing an aortic aneurysm typically involves clinical examination, where the aneurysm can be detected as a pulsating mass in the abdomen. Further confirmation is achieved through ultrasound or CT scans. Routine exams are recommended especially for men aged 65+ years old who are chronic smokers. Other risk factors include those with long-term hypertension and/or heart disease, congenital soft tissue diseases like Ehlers-Danlos Syndrome, and those with a family history of aortic aneurysms and dissections.
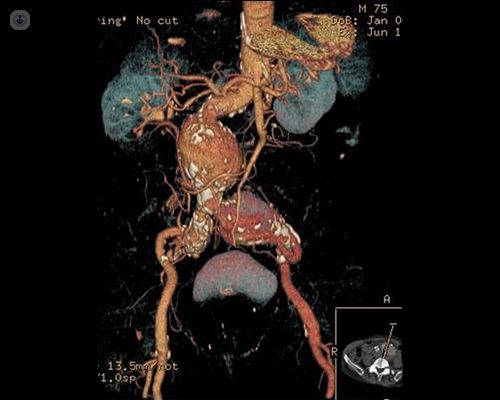
(https://www.topdoctors.co.uk/medical-articles/abdominal-aortic-aneurysm-treatment)
If a small aneurysm is identified, the vascular surgeon will monitor its size and prevent potential complications. For larger aneurysms, surgical intervention or stenting may be necessary, depending on their location and severity, highlighting the importance of early detection and appropriate medical guidance in managing this condition.
Types of Aortic Aneurysms
Aortic aneurysms, abnormal bulges or weaknesses in the aorta, can occur in various regions of the body.
- One common location is in the chest, known as a Thoracic Aortic Aneurysm (TAA).
- In the abdomen, an Abdominal Aortic Aneurysm (AAA) can develop.
- The Thoracoabdominal Aortic Aneurysm (TAAA) spans between the chest and abdomen.
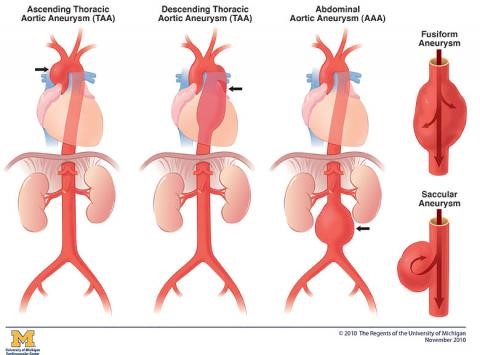
(https://www.uofmhealth.org/conditions-treatments/thoracic-aortic-aneurysm)
These conditions pose serious health risks and may require medical intervention to prevent potentially life-threatening complications.
Treatment Options for Aortic Aneurysm
Treatment options for abdominal aortic aneurysms can be broadly categorized into two main approaches. The first is Open Surgical Repair, a method involving the creation of a long incision on the abdominal wall. While this approach is the traditional method, it comes with high risks due to its invasive nature. Therefore, Open Surgical Repair is typically recommended for fitter patients with lower surgical risk. Recovery after open surgery is an intensive process, often necessitating up to a week of care in the intensive care unit (ICU), and patients typically require about one to six weeks to fully recuperate.
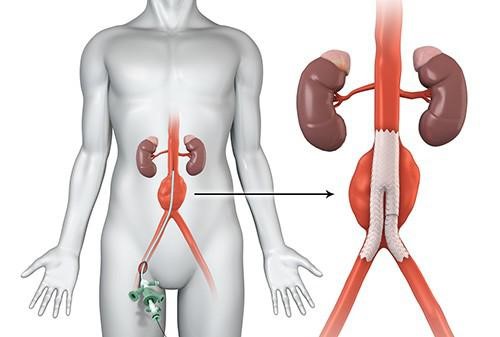
The second approach is Minimally Invasive Repair, specifically EndoVascular Aortic Repair (EVAR), which utilizes covered stent-grafts. In this procedure, specialized stents are inserted through small (approximately 1cm) incisions in the groin, threading them via the femoral arteries to the site of the aneurysm. These stents effectively reline and exclude the aneurysm from the circulation of arterial blood pressure under the guidance of X-ray imaging (fluoroscopy). EVAR is a more suitable option for older patients or those with numerous underlying health conditions, which increase surgical risks. Notably, EVAR can be performed under local anesthesia with mild sedation. Patients who undergo EVAR typically do not require ICU care and can be up and about within eight hours after the procedure, with discharge occurring 48 hours post-surgery in most cases. In select instances, young and healthy patients may even be discharged on the same day, highlighting the minimally invasive nature and quicker recovery associated with this approach.
(https://radiology.wales/evar/)
For the most effective treatment tailored to your specific needs, it is advisable to have a thorough discussion with a vascular surgeon who can assess and guide you through your options. Their expertise will help you make an informed decision regarding the best course of action for your condition.
Risks of an Aortic Aneurysm Surgery
Aneurysm surgery is a life-saving procedure, but it’s crucial to be aware of the potential risks and complications associated with it. These can include bleeding, blood clots, and breathing difficulties, which are common concerns during any surgical intervention. Additionally, surgery may carry the risk of damaging nearby organs, such as the intestines, or it could lead to more serious issues like a heart attack or stroke. Infection can occur in the graft used in the surgery or in other parts of the body, such as the lungs, urinary tract, or abdomen. Kidney failure, nerve damage, and even spinal cord injuries are also possible but relatively rare complications. It’s important to have a detailed conversation with your vascular surgeon about these risks, as their likelihood can vary based on your individual health condition. While surgery is never entirely risk-free, your medical team will prioritize safety and employ every available measure to ensure a safe procedure.
Preparing for Recovery at Home
Consider taking the following steps in advance of your surgery to get ready for your recovery at home:
- Set up a comfortable living space on the first floor to minimise risks, stock up on essential supplies and pre-made meals, ensure that your phone and its charger are easy to access.
- If you live alone, make arrangements for someone to stay with you or help you with your groceries and other needs.
- If you do not have any family or friends in the area who can help you during your recovery, talk to your healthcare provider about getting recommendations for caregiving services.
- Seeking help and assistance during your recovery can help you get better and back to your normal life more quickly and independently.
Lifestyle Considerations for Proper Recovery
To safeguard the investment made in your health through surgery, prioritize your heart and overall well-being by adopting these practices:
- Follow a heart-healthy diet by reducing salt, sugar, and saturated fat intake while staying well-hydrated.
- Engage in appropriate exercise recommended by your vascular surgeon.
- Quit smoking to protect your arteries and overall health.
- Seek support from your provider by managing conditions like high blood pressure, high cholesterol, and diabetes through medication adherence and regular check-ups.
- Consider joining a support group to connect with others in similar situations, aiding in the maintenance of lifestyle changes and providing valuable insights into new resources.
FAQs:
An aortic aneurysm is a condition where a section of the aorta, the body’s main blood vessel, bulges outwards like a balloon. This can occur in the chest (thoracic aneurysm), abdomen (abdominal aortic aneurysm), or between the chest and abdomen (thoracoabdominal aortic aneurysm), and it can lead to severe health complications, especially when it causes aortic dissection, where a tear forms in the aorta’s wall, disrupting blood flow to vital organs.
Various factors can trigger aortic issues, including high blood pressure, genetic conditions like Marfan’s Syndrome, high cholesterol, atherosclerosis, inflammatory diseases, trauma, and smoking. Older men with a history of hypertension or heart disease, individuals with congenital tissue disorders, and those with a family history of aortic problems are at higher risk. Managing these risk factors and making healthy lifestyle choices are crucial for preventing aortic complications.
It is important to take note that symptoms are usually a late presentation indicating impending rupture of the aneurysm, and a Vascular surgeon consult should be sought before any symptoms manifest to have good outcomes. If in the unfortunate event that you experience persistent and severe pain in the chest, abdomen, or lower limbs, a pulsating mass in the abdomen, or the onset of gangrene in the toes, please seek emergency medical attention, as these symptoms may be indicative of an impending aortic aneurysm rupture.
Abdominal aortic aneurysms can be treated through either Open Surgical Repair, which involves invasive incisions and is typically recommended for fitter patients with lower surgical risk but requires a longer recovery period and ICU care, or Minimally Invasive Repair using EndoVascular Aortic Repair (EVAR), which is a more suitable option for older patients or those with higher surgical risks. EVAR is performed with small incisions, allows for quicker recovery, and is often done under local anesthesia. To determine the most effective treatment, it’s crucial to consult a vascular surgeon for personalized guidance and assessment.
To ensure a proper recovery after surgery, it’s essential to adopt a heart-healthy diet, exercise as recommended by your vascular surgeon, quit smoking, manage conditions like high blood pressure and high cholesterol through medication and check-ups, and consider joining a support group for assistance in maintaining lifestyle changes and gaining insights into helpful resources. These practices will help protect your heart and overall well-being, preserving the benefits of your surgical investment.
References
- https://www.cdc.gov/heartdisease/aortic_aneurysm.htm
- https://www.nhlbi.nih.gov/health/aortic-aneurysm/symptoms
- https://www.webmd.com/heart-disease/heart-disease-aortic-aneurysm
- https://medlineplus.gov/ency/article/000162.htm

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
- Tags:
- 主动脉瘤
