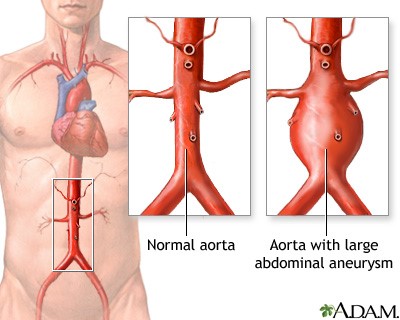
What is an aortic aneurysm?
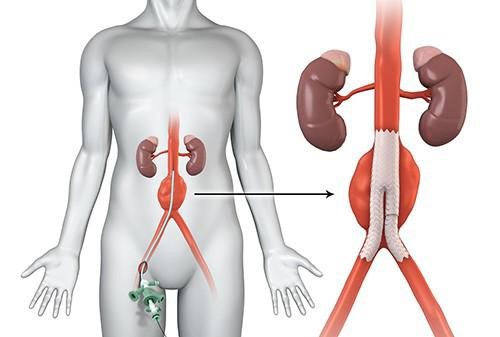
An abdominal aortic aneurysm is a condition in which the aorta, the principal artery of the body that is responsible for transporting oxygen-rich blood from the heart to the lower body, becomes enlarged and bulges outward. This ailment manifests itself largely in the abdominal region. When an aneurysm becomes too large, it presents a serious health risk because the weaker aorta has a greater risk of rupturing, which can result in fatal bleeding. The extent of the aneurysm and the rate at which it is expanding will determine the best course of treatment. Aneurysms may require medical intervention, depending on the severity of the aneurysm and the overall condition of the patient. In some instances, in order to treat an aneurysm without resorting to open surgery, vascular surgeons use a technique known as EndoVascular Aortic Repair (EVAR).
(https://medlineplus.gov/ency/article/000162.htm)
Common Causes of Aortic Aneurysms
A screening test for aortic aneurysms is strongly suggested for people who fit into certain categories of risk factors for the condition. People who regularly smoke cigarettes regularly have a higher chance of developing aneurysms because tobacco use can damage blood vessels, making them more prone to the development of aneurysms. Second, because ageing is a major contributor to the development of aneurysms, people over the age of 65, and especially men, should consider getting screened. People who have a history of hypertension and/or heart disease are also at a higher risk because of the strain that these disorders can exert on the aorta. In addition, people who have congenital soft tissue diseases such as Marfan’s syndrome, Ehlers-Danlos syndrome, or Loeys-Dietz syndrome should be tested, as these abnormalities can cause connective tissues throughout the body, including those in the aorta, to become more fragile. Lastly, having a strong family history of aortic aneurysms and dissections is a significant risk factor. This highlights the importance of undergoing routine screening to identify any potential difficulties as early as possible and successfully manage those that do arise.
(https://gesund.bund.de/en/abdominal-aortic-aneurysm)
Symptoms of an Aortic Aneurysm
Aortic aneurysms are sometimes known as “silent killers” as they usually do not cause any signs or symptoms until a sudden life-threatening rupture occurs. Thus it is imperative that anyone with known risk factors should visit a Vascular surgeon to be screened for the presence of an aortic aneurysm even before there are any signs or symptoms.
If you find yourself experiencing symptoms including persistent and severe pain in areas like the chest or abdomen it should raise immediate concern and it is imperative that you promptly seek emergency medical attention, as these could be signs of an impending aortic aneurysm rupture.
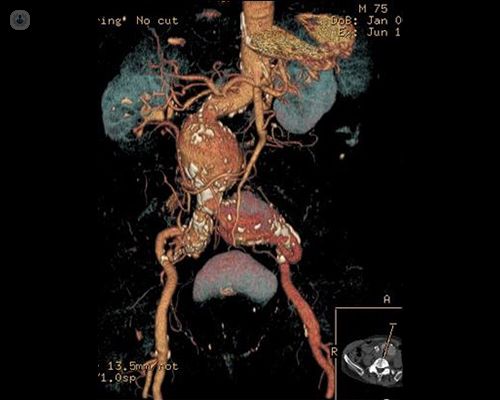
Diagnosis and Tests for Aortic Aneurysm
The diagnosis of an aortic aneurysm typically begins with a clinical examination conducted by a vascular surgeon. During this examination, the doctor may use their hands to carefully feel the abdomen for any abnormalities. In the case of an aortic aneurysm, they may detect a throbbing or pulsating mass in the abdominal area. This pulsation may not always be detected, especially in individuals with a higher BMI as the increased amount of abdominal visceral fat can obscure the pulsation from an enlarged aorta.
While a clinical examination can strongly suggest the presence of an aneurysm, further diagnostic confirmation is crucial. Medical imaging plays a pivotal role in this regard. Two common imaging techniques used to confirm the diagnosis are ultrasound scans and CT (computed tomography) scans.
- An ultrasound is a non-invasive imaging technique that utilizes high-frequency sound waves to create detailed images of the body’s internal structures. This method is widely utilized for initial screening and can provide valuable information about the aneurysm’s characteristics.
- In cases where a more detailed and comprehensive assessment is required, a CT scan may be recommended. This imaging technique combines X-ray technology with computer processing to produce cross-sectional images of the body. A CT scan provides a highly detailed view of the aorta and any aneurysm present, allowing vascular surgeons to assess the size, shape, and exact location of the aneurysm.
(https://www.topdoctors.co.uk/medical-articles/abdominal-aortic-aneurysm-treatment)
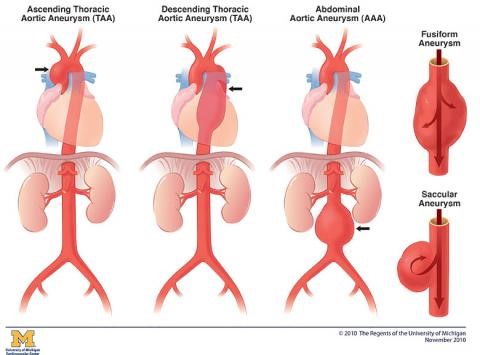
Types of Aortic Aneurysms
The three main regions where aortic aneurysms may occur are the chest (thoracic), the abdomen, and the region between the chest and abdomen (thoracoabdominal). Each of these locations presents unique challenges and potential complications:
- Thoracic Aortic Aneurysm (TAA):
A thoracic aortic aneurysm occurs in the portion of the aorta that runs through the chest. It can involve the ascending aorta (the section that leaves the heart) or the descending aorta (the section that extends through the chest).
2. Abdominal Aortic Aneurysm (AAA):
An abdominal aortic aneurysm occurs in the abdominal portion of the aorta, below the diaphragm. It is one of the most common type of aortic aneurysms.
3. Thoracoabdominal Aortic Aneurysm (TAAA):
A thoracoabdominal aortic aneurysm extends through both the chest and abdominal portions of the aorta. It involves a complex anatomical region.
(https://www.uofmhealth.org/conditions-treatments/thoracic-aortic-aneurysm)
In its early phases, when it is still relatively tiny in size, an aneurysm does not immediately provide a threat to the patient’s health. However, if the aneurysm continues to expand, the walls of the aorta or its lower branches may become thin and lose their ability to stretch. This might cause the aorta to rupture. It is possible that the areas of the wall that have been weakened will no longer be able to withstand the force and pressure of blood flow. It is possible for such an aneurysm to rupture, which would result in serious internal bleeding and ultimately death.
Treatment options for aortic aneurysm
Two primary methods for repairing aortic aneurysms exist: Open Surgical Repair and Minimally Invasive Repair (EndoVascular Aortic Repair or EVAR). Open Surgical Repair is the traditional approach involving extensive abdominal incisions. It’s carries higher morbidity and mortality risks, making it suitable mainly for fitter, lower-risk patients.
In contrast, Minimally Invasive Repair, or EVAR, utilizes covered stent-grafts inserted through small incisions, relining the artery and excluding the aneurysm from blood circulation under X-ray guidance. EVAR is a suitable option for older patients or those with multiple health issues who face greater surgical risks. It can be performed under local anesthesia and mild sedation, typically without the need for ICU care. Patients are often mobile within hours and can be discharged within 48 hours, with some younger and fitter patients even leaving on the same day. The choice between these methods depends on factors like patient age, overall health, and surgical risk.
(https://radiology.wales/evar/)
Procedures for Follow-Up Care After Treatment
After treatment for an aortic aneurysm, continuing follow-up care for the rest of the patient’s life is absolutely necessary. Patients, particularly those who have persistent risk factors such as smoking and hypertension, may develop new aneurysms in various places. It is vital to engage in regular follow-up in order to check for these potential complications and evaluate the integrity of treatments such as endovascular aortic repair (EVAR). This often entails repeated ultrasound and CT scans to detect any difficulties, including leaks around covered stent grafts, and provide timely intervention if it becomes necessary.
Knowing When to Seek Medical Help
It is important to take note that symptoms are usually a late presentation indicating impending rupture of the aneurysm, and a Vascular surgeon consult should be sought before any symptoms manifest to have good outcomes. If in the unfortunate event that you experience persistent and severe pain in the chest, abdomen, or lower limbs, a pulsating mass in the abdomen, or the onset of gangrene in the toes, please seek emergency medical attention, as these symptoms may be indicative of an impending aortic aneurysm rupture.
Benefits of Early Detection and Treatment
The identification of an aortic aneurysm in its early stages carries with it a number of important advantages. It makes it possible for vascular surgeons to intervene in a timely manner, which reduces the risk of the aneurysm becoming larger and maybe rupturing. Second, smaller aneurysms are frequently more receptive to less intrusive treatment alternatives, such as endovascular aortic repair (EVAR), which can lead to speedier recovery times and lower post-operative problems. Third, endovascular aortic repair (EVAR) is a relatively new option that has been shown to be effective. Fourth, early detection enables vascular surgeons to closely monitor the growth of the aneurysm, which ensures that appropriate therapies are initiated whenever necessary. This is especially important for individuals who are at a high risk of experiencing complications from the condition. Lastly, it gives patients the opportunity to make required lifestyle changes to lower the risk of subsequent aneurysm development, eventually improving their long-term health outcomes.
Post-treatment recovery and lifestyle considerations
- Activities – After surgery, rest when needed, prioritize sleep for recovery, and gradually increase walking. Avoid strenuous activities, including heavy lifting, and support your belly when coughing or taking deep breaths.
- Diet – It is important to follow your vascular surgeon’s instructions for your meal plan or diet. Patients sometimes experience changes in appetite that will usually improve as time goes by. It is important to consult your vascular surgeon if no bowel movement occurs after a couple of days.
- Medications – Follow your vascular surgeon’s medication instructions and restart regular medications as advised. Complete prescribed antibiotics and take pain medication as directed. Be cautious with over-the-counter pain medicines and avoid combining them.
- Incision Care – Keep the incision clean and dry to minimize infection risk and ensure proper healing. Follow-up care as recommended is vital for your recovery and safety.
FAQs:
An abdominal aortic aneurysm is the enlargement and bulging of the body’s main artery, the aorta, typically in the abdomen. A larger aneurysm poses a serious risk of rupture, which can be life-threatening. Treatment options vary based on the aneurysm’s size and growth rate, with small, slow-growing aneurysms monitored, and larger ones potentially requiring surgery. Minimally invasive techniques like EndoVascular Aortic Repair (EVAR) may be used to address some aneurysms without major surgery.
Screening for aortic aneurysms is strongly recommended for individuals with specific risk factors. This includes chronic smokers, individuals over 65, particularly males, those with a history of hypertension or heart disease, individuals with congenital soft tissue disorders like Marfan’s syndrome, Ehlers-Danlos syndrome, or Loeys-Dietz syndrome, and those with a strong family history of aortic aneurysms. Routine screening is crucial for early detection and effective management of potential issues.
It is important to take note that symptoms are usually a late presentation indicating impending rupture of the aneurysm, and a Vascular surgeon consult should be sought before any symptoms manifest to have good outcomes. If in the unfortunate event that you experience persistent and severe pain in the chest, abdomen, or lower limbs, a pulsating mass in the abdomen, or the onset of gangrene in the toes, please seek emergency medical attention, as these symptoms may be indicative of an impending aortic aneurysm rupture.
Diagnosing an aortic aneurysm begins with a clinical examination, which can detect a pulsating mass in the abdomen, a crucial indicator. Confirming the diagnosis involves advanced imaging, such as ultrasound and CT scans. Ultrasound offers initial screening, using sound waves to create images showing the aneurysm’s size and location. For more detailed assessments, CT scans provide precise cross-sectional images, aiding treatment decisions.
Two primary methods for repairing aortic aneurysms exist: Open Surgical Repair involves extensive abdominal wall incisions, suitable mainly for fitter, lower-risk patients, but with higher morbidity and recovery times. In contrast, Minimally Invasive Repair (EVAR) uses covered stent-grafts through small groin incisions, suitable for older or higher-risk patients, with shorter recovery times.
References
- www.cdc.gov/heartdisease/aortic_aneurysm.htm
- https://www.nhlbi.nih.gov/health/aortic-aneurysm/symptoms
- https://www.webmd.com/heart-disease/heart-disease-aortic-aneurysm
- https://medlineplus.gov/ency/article/000162.htm

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
- Tags:
- 主动脉瘤
