Introduction to Gangrene: What is Gangrene and How Can it Affect You?
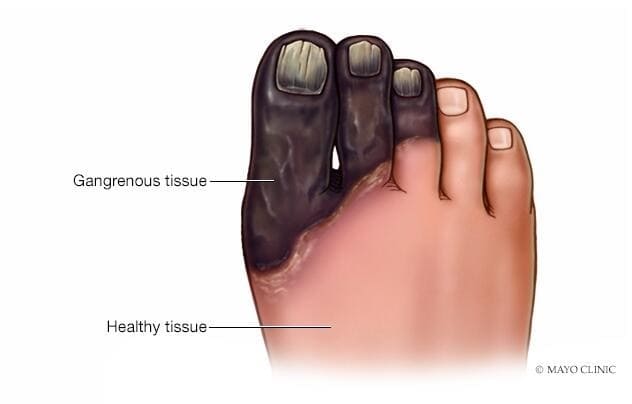
Gangrene is a severe and potentially fatal medical condition that arises when blood flow to a specific area of tissue is obstructed, leading to tissue decay and death. This often manifests as a greenish-black discoloration of the affected skin. Gangrene can result from a combination of factors, including poor circulation and bacterial infection, and it primarily affects the limbs but can also occur internally and spread systemically. Timely diagnosis and treatment are crucial for a successful recovery, making it imperative to understand how to prevent gangrene in the first place.
(https://www.mayoclinic.org/diseases-conditions/gangrene/symptoms-causes/syc-20352567)
Causes of Gangrene: Identifying the Risk Factors
Gangrene can be attributed to three primary causes, often exacerbated by underlying health conditions. Firstly, inadequate circulation is a major factor, as it starves body cells of essential oxygen and nutrients over time, ultimately resulting in tissue death. Secondly, bacterial infections play a critical role, particularly in untreated wounds where bacteria multiply, produce harmful toxins and gas, and contribute to tissue demise, a condition known as gas gangrene. Lastly, traumatic injuries, especially those that create deep and sizable wounds, create an entry point for bacteria. Without prompt treatment, these infections can progress to gangrene.
(https://www.linkedin.com/posts/dharmesh-davra-642914169_gangrene-vascularproblems-gangreneriskfactors-activity-7053607874391941120-ZpHS)
Types of Gangrene: Knowing the Differences
Gangrene encompasses various types, each requiring immediate treatment to prevent potentially fatal progression:
- Dry gangrene, common in individuals with conditions like diabetes or atherosclerosis, results in dry, shriveled, and discolored skin.
- Wet gangrene involves bacterial infection, leading to blistering, swelling, and pus formation, often seen in diabetic patients with neuropathy.
- Gas gangrene affects deep tissues and internal organs, initially unnoticed but progressing to skin discoloration and gas accumulation, which can be deadly.
- Internal gangrene occurs in organs like the intestines due to reduced blood flow, often from conditions like hernias or twisting intestines.
- Fournier’s gangrene, rare and more common in men, affects the genital or urinary tract. Swift treatment is essential for all these forms of gangrene.
Diagnosing Gangrene: How to Recognize the Symptoms
Gangrene exhibits distinct symptoms based on its type. In dry gangrene, affected areas display shriveled skin, pain, and cold, hard, and numb skin. Conversely, wet gangrene manifests through skin discoloration ranging from red to black, a visible boundary between healthy and damaged skin, blisters with pus, swelling, pain, fever, and even a crackling noise when the skin is touched. If the infection spreads, it can lead to septic shock, marked by confusion, low blood pressure, lightheadedness, fever, a rapid heart rate, and shortness of breath.
Complications of Gangrene: Understanding the Risk Factors for Complications
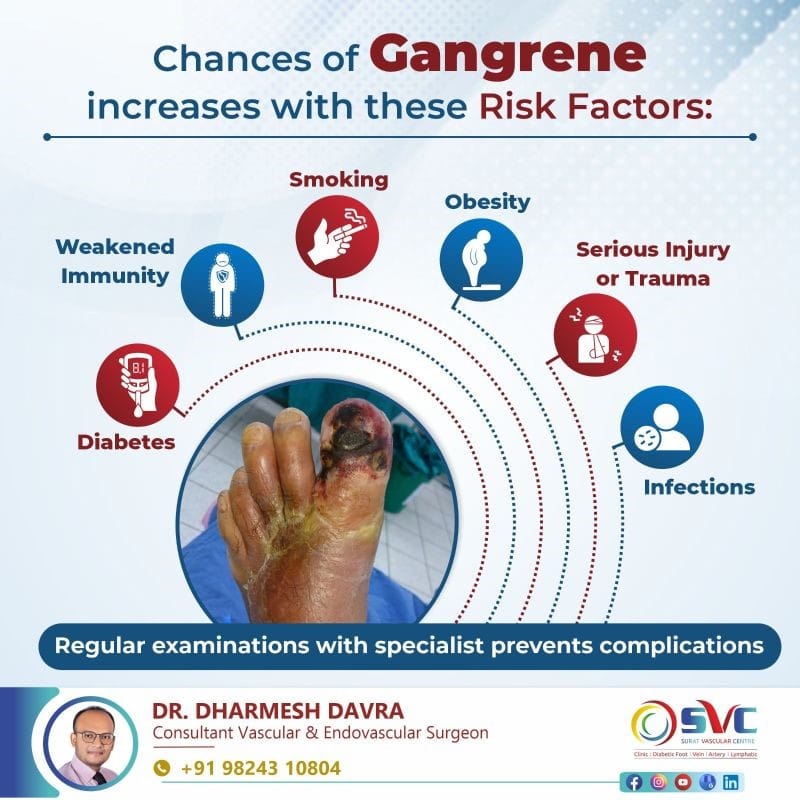
Several risk factors contribute to the development of gangrene. Diabetes poses a significant risk as it can damage nerves in the extremities, leading to unnoticed injuries and poor wound care, creating an environment for gangrene to thrive. High blood sugar levels in diabetes also contribute to arteriosclerosis, which hinders blood flow, exacerbating the risk. Additionally, diabetes can weaken the immune system, making individuals more susceptible to infections. Narrowed arteries, atherosclerosis, and peripheral artery disease all restrict blood flow, depriving tissues of vital oxygen and nutrients.
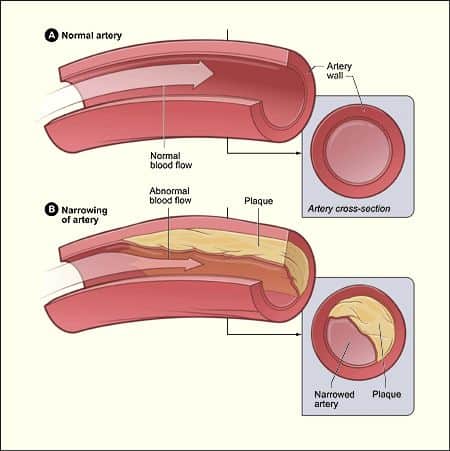
(https://www.nhlbi.nih.gov/health/atherosclerosis)
Smoking promotes atherosclerosis and arterial hardening, further compromising circulation. Serious frostbite can reduce circulation in affected areas, while obesity often leads to vascular-related conditions like diabetes and atherosclerosis, increasing gangrene risk. Raynaud’s phenomenon, characterized by narrowed blood vessels in the fingers, can also lead to oxygen deprivation and gangrene. Finally, immunosuppression weakens the immune system’s infection-fighting abilities, heightening the risk of gangrene development. Understanding and managing these risk factors is crucial for preventing gangrene, especially for those with diabetes.
Diagnosis for Gangrene
Diagnosing gangrene involves recognizing the characteristic purplish-black tissue color and the loss of function and sensation in the affected body part. To determine the severity and guide treatment, various tests are conducted. Blood tests analyze for signs of infection, such as an elevated white blood cell count indicating bacterial presence. Imaging tests like CT scans, MRI scans, and X-rays assess infection spread, including gas under the skin, a potential indicator of deadly gas gangrene. Simultaneously, blood vessel scans check for blockages contributing to gangrene. Additionally, cultures are performed, including blood cultures to identify bacteria accurately and assess antibiotic susceptibility, as well as tissue/fluid cultures to pinpoint the specific bacteria responsible for the infection, aiding in appropriate antibiotic prescription.

(https://www.researchgate.net/publication/51114139_Gas_gangrene_and_osteomyelitis_of_the_foot_in_a_diabetic_patient_treated_with_tea_tree_oil/figures?lo=1)
Treatment Options for Gangrene: What are the Non-Surgical and Surgical Options?
- Antibiotics are commonly prescribed to combat bacterial infections, administered via IV drips or tablets, depending on the infection’s severity.
- Debridement surgery involves thorough wound cleaning and the surgical removal of dead tissue to promote healing, often accompanied by antibiotic therapy.
- Angioplasty and stenting procedures restore proper blood flow to supply oxygen and nutrients to affected tissues.
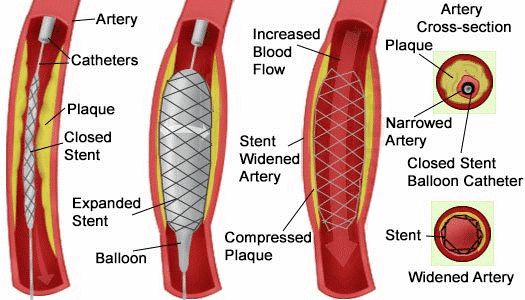
(https://coastalvascular.net/treatments/stenting/)
4. Open bypass surgery bypasses blocked blood vessels using grafts to restore circulation.
5. In severe cases, amputation may be necessary to prevent gangrene spread, followed by prosthetic limb fitting and physiotherapy.
Post-surgery, Vacuum-Assisted Closure (VAC) devices accelerate healing by creating a conducive environment, removing excess fluids, and drawing wound edges together for faster recovery. This comprehensive approach helps individuals recover from gangrene more swiftly.

(https://www.3m.co.uk/3M/en_GB/Medical-GB/products/negative-pressure-wound-therapy/)
Prevention of Gangrene: Practicing Good Hygiene and Taking Necessary Precautions
To prevent gangrene and maintain healthy blood flow, especially if you have risk factors like peripheral artery disease or diabetes, focus on a heart-healthy diet, regular exercise, blood glucose control, and learning about diabetes-related leg and foot complications. Quit smoking and always protect your feet, never going barefoot outdoors. Practice proper toenail care, daily foot hygiene, and wear well-fitting socks and shoes. Regularly check your feet for injuries or skin issues and have your provider examine them during appointments. These steps are crucial for safeguarding your vascular health and preventing gangrene.
Diabetes and Gangrene Prevention: Protect Your Feet and Vascular Health
For individuals with diabetes, maintaining foot health is crucial. Annual foot check-ups are recommended, with more frequent checks if additional complications are present. Daily self-examinations for numbness, cuts, swelling, or skin issues are essential. Properly fitting shoes and socks can reduce skin trauma. Weight management is vital to mitigate diabetes-related vascular damage, and smoking cessation is imperative to avoid atherosclerosis and the risk of gangrene. Wound care, alcohol moderation, and regular exercise further support overall vascular health, enhancing blood circulation and reducing gangrene risk.

(https://www.diabetes.co.uk/foot-care/foot-checks.html)
When to Seek Medical Attention for Gangrene
It’s essential to maintain regular checkups with your vascular surgeon, especially if you possess risk factors associated with gangrene, like peripheral artery disease. In cases where you exhibit signs or symptoms of gangrene, or experience symptoms indicative of septic shock, immediate medical attention is imperative. Signs of septic shock encompass a rapid yet feeble pulse, confusion or disorientation, dizziness upon standing, cold and clammy pale skin, breathing difficulties, and nausea.
Final Words
Gangrene is a severe medical condition caused by obstructed blood flow to tissue, resulting in tissue decay and death, often characterized by greenish-black skin discoloration. It can stem from poor circulation, bacterial infection, or traumatic injuries, affecting limbs and internal organs. There are various types of gangrene, each requiring immediate treatment, including dry gangrene, wet gangrene, gas gangrene, internal gangrene, and Fournier’s gangrene. Symptoms vary depending on the type but can include pain, skin discoloration, blisters, swelling, and even septic shock in severe cases. Consulting with a vascular surgeon is crucial when dealing with gangrene as they specialize in diagnosing and treating vascular issues, which are often at the root of gangrene. Their expertise is essential for determining the best course of action to improve blood flow and prevent further tissue damage.
FAQs:
Gangrene is a life-threatening condition caused by blocked blood flow, leading to tissue decay and often resulting in greenish-black skin discoloration. It primarily affects limbs and internal organs, with prompt diagnosis and treatment being crucial for recovery and prevention.
Gangrene symptoms vary by type; dry gangrene involves pain and shriveled, numb skin, while wet gangrene exhibits skin discoloration, blisters, and swelling, potentially progressing to septic shock if untreated.
Treatment options for gangrene include antibiotics, debridement surgery, angioplasty, bypass surgery, and in severe cases, amputation, followed by post-surgery measures like Vacuum-Assisted Closure (VAC) devices.
Consulting a vascular surgeon is essential for gangrene management, as they specialize in vascular issues, which are often the underlying cause.
Preventing gangrene involves a healthy lifestyle, especially for those with risk factors like diabetes or peripheral artery disease, including proper foot care, smoking cessation, and regular medical checkups.
References:
[1] https://www.sgvascularctr.com/what-is-a-gangrene/
[2] https://www.sgvascularctr.com/gangrene-diagnosis-and-treatment/
[3] https://my.clevelandclinic.org/health/diseases/21070-gangrene
[4] https://www.sgvascularctr.com/living-with-diabetes-how-to-prevent-gangrene/

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
- Tags:
- How To Prevent Gangrene
