This guide aims to provide answers to common questions about varicose veins from the viewpoint of a vascular surgeon. Whether you have varicose veins, are at risk of developing varicose veins, or want to learn more about this condition, this guide is perfect for you.
What are Varicose Veins?
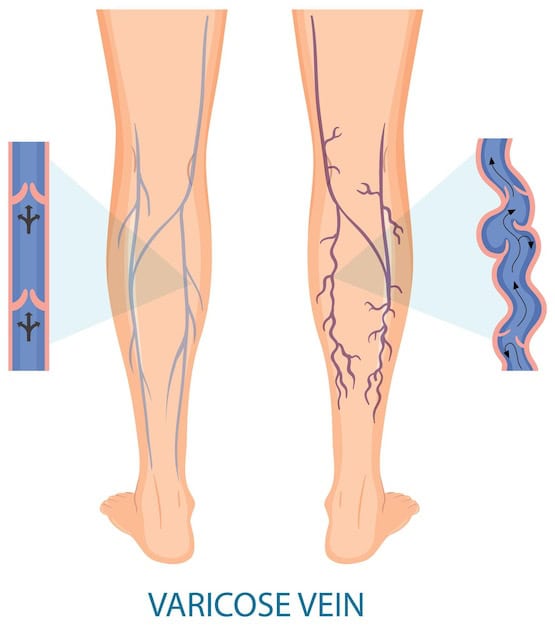
Varicose veins are swollen and enlarged blood vessels that can lead to discomfort and pain for those affected. They are often associated with a milder form known as spider veins. Although varicose veins can appear anywhere in the body, they commonly occur in the legs, primarily due to the increased pressure in the lower body when standing and walking upright.
These visible veins result from a malfunction in the valves within the blood vessels. These valves, usually responsible for ensuring one-way blood flow, weaken and fail. Consequently, blood flows backward and accumulates in the veins, rather than progressing efficiently toward the heart. This abnormal flow leads to the veins becoming congested, twisting, and stretching, giving rise to varicose veins.

(image source: https://www.medicalnewstoday.com/articles/240129)
What Are the Signs or Symptoms of Varicose Veins?
- Varicose veins are characterized by veins in your legs that appear swollen and enlarged. They can often be seen through the skin and may have a twisted or bulging appearance. These veins can take on various colors, such as red, purple, or blue, which makes them stand out.
- People with varicose veins often experience a sensation of heaviness in their legs. It can feel as though your legs are weighed down or swollen. This discomfort is often most noticeable after standing or sitting for extended periods.
- A common symptom of varicose veins is aching or pain in the legs. This discomfort may vary from mild to moderate and can be persistent or intermittent. It’s often linked to the pressure and strain placed on the affected veins.
- Over time, the skin around varicose veins may undergo changes. You might notice that the skin in the affected area becomes discolored, taking on a darker hue. This change in skin color is a result of blood pooling in the affected veins and can be particularly noticeable in fair-skinned individuals.
- Itching is another symptom that some people with varicose veins experience. The skin around the affected veins can become irritated and itchy. Scratching should be avoided as it can worsen skin problems and potentially lead to complications.
(image source: https://www.freepik.com/free-vector/human-legs-with-varicose-vein_28768312.htm)
What Causes Varicose Veins?
- Varicose veins become more common as people grow older. This is because, over time, the valves inside the veins can wear out. These valves usually help blood flow upwards towards the heart, but when they weaken or become damaged, blood can flow backward and pool in the veins, leading to varicose veins.
- Varicose veins tend to affect more women than men. This gender difference is linked to hormonal changes. Hormonal shifts that occur during pregnancy, before menstruation, or during menopause can relax the walls of the veins, making them more prone to becoming varicose.
- When a woman is pregnant, her body produces more blood to nourish both herself and the growing fetus. This increased blood volume puts extra pressure on the veins. To accommodate this, the veins enlarge to support the added blood flow.
- Your family tree can play a significant role in your risk of developing varicose veins. If your parents or close relatives have had varicose veins, you’re more likely to get them too. It’s almost like having a genetic blueprint that increases your chances of experiencing this condition.
- Being overweight places extra pressure on your veins, especially those in your legs. This added pressure makes it harder for your veins to effectively push blood back up to the heart. Think of it as a heavy backpack weighing down on your veins, making their job more challenging.
- If your job or daily routine requires you to stand for long hours, this can lead to varicose veins. When you stand for extended periods, it can be more difficult for your veins to efficiently move blood against gravity. It’s like asking your veins to work extra hard without getting a break, which can result in poor blood flow.

(image source: https://www.healthline.com/health/doppler-ultrasound-exam-of-an-arm-or-leg)
How Can Vascular Surgeons Help Patients with Varicose Veins?
- Vascular surgeons are skilled in diagnosing varicose veins through clinical examinations and specialized tests like ultrasound scans. They assess the underlying causes of the condition, which helps determine the most appropriate treatment plan.
- Once the diagnosis is established, vascular surgeons work with patients to develop a personalized treatment plan. They consider factors like your condition and lifestyle to recommend the best course of action.
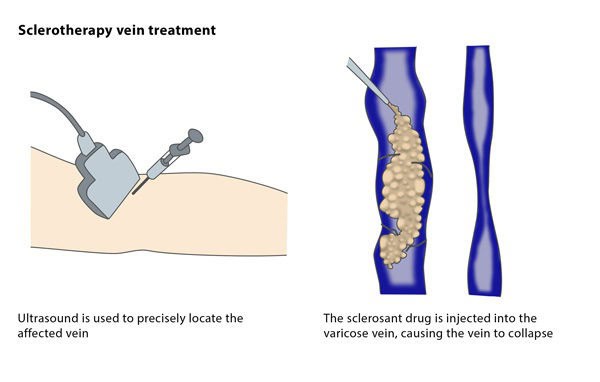
- Vascular surgeons are trained in performing minimally invasive procedures to treat varicose veins. These procedures, such as radiofrequency ablation and sclerotherapy, can effectively close off or remove veins, alleviating symptoms and improving the appearance of the legs.
- In cases where varicose veins are severe or have complications, surgical intervention may be necessary. Vascular surgeons can perform surgical procedures like vein ligation and stripping to remove problematic veins and improve blood circulation.
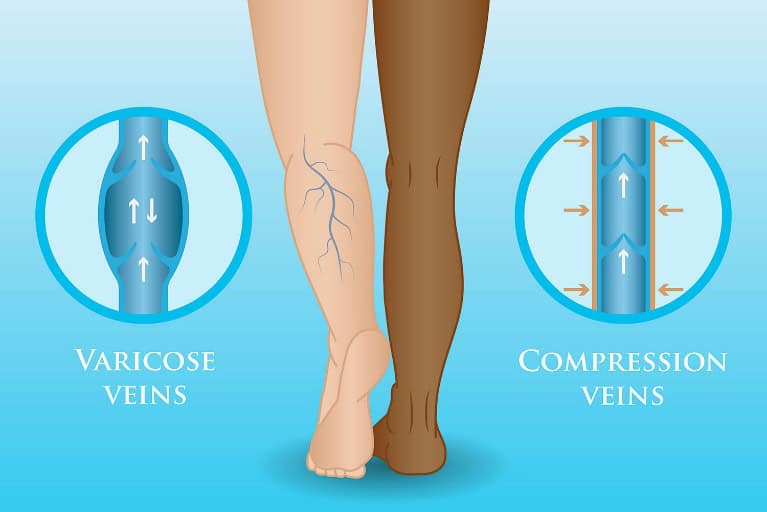
- Vascular surgeons educate patients about varicose vein prevention and lifestyle modifications. They also provide advice on wearing compression stockings, which can improve blood flow in the legs.
How Do Vascular Surgeons Diagnose Varicose Veins?
You will undergo a clinical physical assessment during which a vascular surgeon will carefully examine your legs. During this evaluation, they will observe for any visible signs such as swollen or twisted veins, assess for changes in skin color or texture, and inquire about any discomfort or pain you may be experiencing. Think of this as an initial check where the vascular surgeon collects information to spot the presence of varicose veins and other related issues.
An ultrasound scan uses sound waves to generate images of the inside of your body. In the case of varicose veins, the focus of the ultrasound scan is on your legs. In this procedure, a technician or sonographer will apply a unique gel to your legs and utilize a device known as an ultrasound transducer to emit and receive sound waves. These waves bounce off the blood vessels in your legs, producing detailed images visible on a screen. With the help of an ultrasound scan, your vascular surgeon will be able to visualize blockages or areas of weak valves that hinder blood flow.
(image source: https://www.cirse.org/patients/general-information/ir-procedures/sclerotherapy/)
What Are the Conservative Non-Surgical Treatment Options for Varicose Veins?
One of the primary conservative treatments for varicose veins involves wearing tight compression stockings. These stockings are specially designed to provide graduated compression, meaning they are tighter at the ankle and gradually become looser as they move up the leg. Compression stockings exert gentle pressure on the leg veins. This pressure encourages blood to flow upwards towards the heart. In varicose veins, the valves in the veins may not work properly, causing blood to pool or flow backward. Compression stockings assist in counteracting this by aiding blood circulation.
By improving blood flow, compression stockings can alleviate common symptoms associated with varicose veins, such as leg swelling, aching, and heaviness. In the early stages of varicose veins or in cases with milder symptoms, wearing compression stockings can effectively manage the condition and prevent it from getting worse. They are often recommended as a first-line treatment, especially when the veins are not severely damaged. However, it’s important to note that while compression stockings can provide relief and prevent further deterioration in some cases, they do not eliminate varicose veins.
(image source: https://www.veinhealth.com.au/compression-stockings-can-help-your-varicose-veins/)
What Are the Surgical Treatment Options for Varicose Veins?
Traditional open surgery for treating varicose veins is commonly referred to as “high-tie ligation and vein stripping.” This surgical approach involves a few key aspects. Firstly, it typically necessitates the administration of general anesthesia, meaning the patient is put to sleep during the procedure. Secondly, open surgery for varicose veins usually requires an overnight stay in the hospital for post-operative monitoring and care. While this surgical method can effectively treat varicose veins, it is often linked to certain drawbacks.
In some cases, patients experience post-operative pain which can make the recovery period more uncomfortable for patients. Additionally, the process of open surgery tends to be slower in comparison to minimally invasive procedures, and it may result in more extended downtime for the individual. Consequently, many patients and vascular surgeons explore less invasive treatment options, such as sclerotherapy or radiofrequency ablation, to achieve varicose vein relief with fewer complications and a quicker recovery.
What Are Minimally Invasive Treatments for Varicose Veins?
Minimally invasive procedures offer similar benefits to traditional surgery but with less pain and a faster recovery. These procedures involve small incisions and methods in technology that allow for vein sealing through probes inserted into the vein. They are typically performed as day surgery, minimizing disruption to daily life and eliminating the need for a hospital stay. These techniques include Radio Frequency Ablation (RFA) for heating and damaging the vein wall, Venseal™/VenaBlock Glue Closure for sealing varicose veins with medical adhesive, Clarivein™ Mechanochemical Ablation for mechanical destruction and chemical sealing, and Cryo-Laser and Cryo-Sclerotherapy (CLaCs) for spider veins using laser and sclerotherapy under skin cooling, leaving minimal scarring. The specific treatment for you ultimately depends on the instructions of your vascular surgeon.
How Does Radio Frequency Ablation Work?
Radio Frequency Ablation uses radiofrequency energy to generate controlled heat. This energy is used to damage the vein wall. This targeted thermal energy causes the affected veins to close and redirect blood flow to healthier veins nearby. RFA is known for its efficiency and safety, typically completed within a relatively short timeframe of about 35-40 minutes, and it is performed on an outpatient basis, meaning patients can usually return home the same day.
How Does Venseal/VenaBlock Glue Closure Work?
The Venseal™/VenaBlock Glue Closure procedure involves the application of a specially formulated medical adhesive to permanently seal varicose veins. By closing off these problematic veins, the blood is redirected to healthier neighboring veins, offering relief from the condition. This treatment is known for its comfort and efficiency, typically taking only 15-20 minutes to complete.
How Does Clarivein Mechanochemical Ablation Work?
In the Clarivein™ Mechanochemical Ablation procedure, a unique approach combines the mechanical disruption of veins with the injection of sclerosant, a chemical used in sclerotherapy to close off veins. A specialized catheter with a rapidly rotating wire is inserted, effectively damaging the innermost vein layer (venous intima). Simultaneously, a controlled injection of sclerosant is administered to seal the vein. This technique is painless and necessitates fewer local anesthesia injections. Importantly, the mechanochemical ablation method carries no risk of heat-induced damage to nearby nerves, enhancing its safety profile.
Where Can I Find a Vascular Surgeon in Singapore?
The Vascular & Interventional Centre in Singapore offers minimally invasive treatment for varicose veins. Our vascular surgeons are well-trained in screening, diagnosing, and treating this condition. To find out if the procedure is right for you, you may request a consultation so you can understand your options and choose the best treatment for you. You can contact us at +65 6694 6270 during clinic hours or you can send an e-mail to en*****@sg***********.com.
FAQs:
The cost of varicose vein treatment in Singapore varies depending on the provider and the specific treatment chosen, so it’s best to schedule a consultation to get an accurate estimate.
Whether varicose vein treatment is covered by insurance depends on your insurance policy and the medical necessity criteria set by your provider. You should check with your insurance company to determine coverage.
To prevent varicose veins, you can engage in regular exercise, maintain a healthy weight, elevate your legs, when possible, avoid prolonged sitting or standing, and wear compression stockings if recommended by a vascular surgeon.
If varicose vein treatment has not provided the desired results, it’s essential to consult with your vascular surgeon to discuss alternative treatment options or further evaluation.
Maintaining the results of varicose vein treatment involves following post-treatment instructions, wearing compression stockings if advised, staying active, maintaining a healthy lifestyle, and attending follow-up appointments.
References:
- https://www.healthline.com/health/varicose-veins
- https://www.sgvascularctr.com/service/vein-diseases-varicose-veins/
- https://www.sgvascularctr.com/wp-content/uploads/2022/01/spider-and-varicose-veins-1.pdf

Dr Chen Min Qi profile
Dr. Chen Min Qi is a fellowship-trained Vascular and Endovascular Surgeon who graduated from the National University of Singapore in 2005. He subsequently completed his basic and advanced training in General and Vascular Surgery while obtaining the Member of Royal College of Surgeons of Edinburgh (MRCSed) qualification in 2010, and the Master of Medicine (General Surgery) qualification in 2015. Dr Chen was subsequently successful at the fellowship exams obtaining the Fellow of Royal College of Surgeons of Edinburgh (FRCSed) qualification in 2016.
Upon completion of his advanced surgical training, Dr Chen Min Qi joined the newly opened Ng Teng Fong General Hospital (NTFGH) as a specialist in the Vascular Surgery division. In 2018, Dr Chen was awarded the Health Manpower Development Plan (HMDP) grant from MOH to undergo further subspeciality Vascular training at the internationally renowned St Mary’s Hospital in London, United Kingdom. There Dr Chen gained further experience in surgeries on complex abdominal and thoracoabdominal aortic aneurysms, redo open repair of abdominal aortic aneurysms following failed EVAR surgeries as well as carotid endarterectomy surgery and lower limb revascularization surgeries.
Upon his return in 2020, Dr Chen Min Qi joined the newly formed Woodlands Health as head of their Vascular service, before joining his current practice at the Vascular and Interventional Centre in January 2023.
- Tags:
- Treatment of varicose veins
- Treatment of varicose veins Singapore
- varicose vein specialist Singapore
- Varicose veins
- Varicose Veins Doctor Singapore
- Varicose veins in legs Singapore
- Varicose veins pregnancy Singapore
- varicose veins procedure singapore
- Varicose Veins Singapore
- Varicose veins surgery
- Varicose veins surgery Singapore
- varicose veins treatment
- varicose veins treatment singapore
